Comparing Chancroid and Herpes: What Are the Differences?

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Dr. Aditi completed her undergraduate medical education at AJIMS, Mangalore, after which she worked in multi-speciality hospitals with COVID patients and in the Pain and Palliative medicine department. Driven by her experiences, she developed a keen interest in psychiatry. Dr. Aditi believes that mental health is just as, if not more important, than physical health.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 17 February, 2024
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
When it comes to sexually transmitted infections (STIs), there are a variety of diseases that individuals may come across. Chancroid and herpes are two such STIs that can cause similar symptoms but have their unique differences. It’s important to understand these differences to seek appropriate treatment and take preventative measures. In this article, we’ll delve deeper into chancroid and herpes, and explore what sets them apart.
What Is Chancroid?
Chancroid is a bacterial infection that primarily affects the genital area. It is caused by the bacterium Haemophilus ducreyi. Chancroid is a sexually transmitted infection (STI) and is characterized by the development of painful genital ulcers or sores. The condition is more common in certain parts of the world, particularly in sub-Saharan Africa and parts of Asia.
Here are some key details about chancroid:
- Causing Agent:
- Chancroid is caused by the bacterium Haemophilus ducreyi.
- The infection is primarily transmitted through sexual contact, including vaginal, anal, and oral sex.
- Symptoms:
- The hallmark symptom of chancroid is the development of one or more painful, open sores or ulcers in the genital area. These ulcers may be soft, shallow, and have a sharply defined border.
- The sores may bleed or produce a purulent (pus-like) discharge.
- Other symptoms may include painful urination, painful or swollen lymph nodes in the groin, and in some cases, flu-like symptoms.
- Incubation Period:
- The incubation period for chancroid is typically 3 to 10 days after exposure to the bacterium.
- Diagnosis:
- Chancroid is diagnosed based on clinical examination, medical history, and laboratory tests.
- Laboratory tests may include the identification of the bacteria through cultures or nucleic acid amplification tests (NAATs).
- Complications:
- If left untreated, chancroid can lead to complications such as the formation of abscesses and the development of permanent scars.
- Chancroid may also increase the risk of acquiring and transmitting other sexually transmitted infections, including HIV.
It’s important to note that chancroid is relatively rare in many parts of the world, and its prevalence can vary. Early detection and appropriate medical treatment are essential for managing the infection and preventing complications. Individuals experiencing symptoms suggestive of chancroid should seek medical attention for diagnosis and treatment.

Chancroid Symptoms And Causes
Symptoms of Chancroid:
- Genital Ulcers:
- The primary symptom of chancroid is the development of one or more genital ulcers or sores.
- These ulcers are typically painful and may be described as soft, shallow, and have a well-defined border.
- The ulcers can vary in size and are often accompanied by a base of inflamed tissue.
- Pain and Discomfort:
- Individuals with chancroid often experience pain or discomfort at the site of the ulcers.
- Pain may range from mild to severe, and it can interfere with daily activities.
- Purulent Discharge: The ulcers may produce a purulent (pus-like) discharge, and there may be crusting or bleeding.
- Painful Lymph Nodes:
- Swelling and tenderness of the lymph nodes in the groin area (inguinal lymphadenopathy) are common.
- Enlarged lymph nodes may be felt as lumps in the groin and can be quite painful.
- Painful Urination: Some individuals with chancroid may experience pain or discomfort during urination.
- Flu-Like Symptoms: In some cases, individuals may develop flu-like symptoms, such as fever, fatigue, and body aches.
Causes of Chancroid:
- Bacterial Infection:
- Chancroid is caused by the bacterium Haemophilus ducreyi.
- This bacterium is responsible for the development of the characteristic genital ulcers associated with the infection.
- Transmission:
- Chancroid is primarily transmitted through sexual contact, including vaginal, anal, and oral sex.
- The bacterium enters the body through small breaks in the skin or mucous membranes during sexual activity.
- Incubation Period:
- The incubation period, or the time from exposure to the bacterium to the development of symptoms, is typically 3 to 10 days.
- Risk Factors:
- Risk factors for chancroid include engaging in unprotected sexual activity with an infected individual.
- Individuals with multiple sexual partners or those with a history of other sexually transmitted infections may be at an increased risk.
- Geographic Prevalence: Chancroid is more common in certain regions of the world, including sub-Saharan Africa and parts of Asia, but it can occur in other areas as well.
- Complications:
- If left untreated, chancroid can lead to complications such as the formation of abscesses and scarring in the genital area.
- Chancroid may also increase susceptibility to and transmission of other sexually transmitted infections, including HIV.
- Diagnosis:
- Diagnosis is typically based on clinical examination, medical history, and laboratory tests.
- Laboratory tests may include the identification of Haemophilus ducreyi through cultures or nucleic acid amplification tests (NAATs).
It’s important for individuals experiencing symptoms suggestive of chancroid to seek prompt medical attention for diagnosis and treatment. Practicing safe sex and maintaining open communication with sexual partners can also help prevent the transmission of chancroid and other sexually transmitted infections.
Chancroid Treatments
Chancroid, being a bacterial infection, is typically treated with antibiotics. Here are the details of the treatments for chancroid:
Antibiotic Therapy:
- Azithromycin:
- Azithromycin is a commonly prescribed antibiotic for chancroid.
- A single oral dose is often effective in treating the infection.
- Ceftriaxone:
- Ceftriaxone, another antibiotic, may be used as an alternative treatment for chancroid.
- It is often administered as a single injection.
- Erythromycin:
- Erythromycin is an alternative antibiotic option, especially in cases where azithromycin or ceftriaxone cannot be used.
- It is administered orally and may require a longer course of treatment.
- Dual Therapy:
- In some cases, a combination of antibiotics may be prescribed for enhanced effectiveness.
- For example, a healthcare provider might prescribe a single dose of azithromycin along with a course of ceftriaxone.
Treatment Considerations:
- Prompt Treatment: Early and prompt treatment is crucial to prevent complications and reduce the risk of transmission to others.
- Follow-Up Testing: After completing the antibiotic treatment, follow-up testing may be recommended to ensure that the infection has been successfully eradicated.
- Partner Notification: Individuals diagnosed with chancroid should inform their sexual partners about the infection so that they can seek testing and treatment if necessary.
- Abstaining from Sexual Activity: During the course of treatment and until the sores have healed completely, individuals are advised to abstain from sexual activity to avoid spreading the infection.
- Avoiding Alcohol and Irritants: Individuals being treated for chancroid may be advised to avoid alcohol and other irritants that can exacerbate the healing process.
- Pain Management: Pain associated with chancroid ulcers can be managed with pain relievers such as acetaminophen or ibuprofen.
Monitoring and Follow-Up:
- Resolution of Symptoms: Improvement in symptoms, including the healing of ulcers, is typically observed within a few days of starting antibiotic treatment.
- Follow-Up Visits: Follow-up visits with a healthcare provider are important to monitor progress and ensure complete resolution of the infection.
- Preventing Recurrence: Practicing safe sex, including the use of condoms, is essential to prevent the recurrence of chancroid and other sexually transmitted infections.
Complications:
If left untreated, chancroid can lead to complications such as the formation of abscesses, scarring, and an increased risk of acquiring and transmitting other sexually transmitted infections, including HIV. Prompt and appropriate treatment is crucial to minimize the risk of complications.
It’s important for individuals who suspect they have chancroid or are experiencing symptoms to seek medical attention promptly. Only a healthcare provider can diagnose the infection and prescribe the appropriate antibiotics for effective treatment.
Chancroid Prevention
Preventing chancroid involves practicing safe sex and taking measures to reduce the risk of acquiring or transmitting the infection. Here are detailed preventive measures for chancroid:
- Safe Sex Practices: Consistent and correct use of latex or polyurethane condoms can significantly reduce the risk of sexually transmitted infections, including chancroid. Condoms act as a barrier, preventing direct skin-to-skin contact and the exchange of bodily fluids.
- Reducing Sexual Partners: Limiting the number of sexual partners can reduce the risk of exposure to sexually transmitted infections, including chancroid.
- Screening and Testing: Regular screening and testing for sexually transmitted infections are essential, especially for individuals with multiple sexual partners or those at an increased risk. Early detection allows for prompt treatment and reduces the risk of complications.
- Partner Communication: Open and honest communication with sexual partners is crucial. Individuals diagnosed with chancroid or other sexually transmitted infections should inform their partners so that they can seek testing and treatment as needed.
- Avoiding High-Risk Behaviors: Avoiding high-risk sexual behaviors, such as unprotected sex and engaging in sexual activities with individuals of unknown or high-risk sexual health status, can help prevent the transmission of chancroid.
- Education and Awareness: Educating oneself and others about sexually transmitted infections, their symptoms, and preventive measures is important. Knowledge empowers individuals to make informed decisions about their sexual health.
- Regular Health Check-ups: Regular visits to healthcare providers for routine check-ups and screenings can help monitor overall sexual health and detect any potential infections early.
- Vaccination: At present, there is no specific vaccine for chancroid. But, staying up-to-date with vaccinations for other sexually transmitted infections, such as human papillomavirus (HPV) and hepatitis B, is important for overall sexual health.
- Preventing Recurrence: Individuals who have been treated for chancroid should follow their healthcare provider’s advice regarding abstaining from sexual activity until the sores have healed completely. Practicing safe sex thereafter is essential to prevent recurrence.
- Avoiding Irritants: Practices such as avoiding irritants, including certain personal hygiene products or substances that may exacerbate genital irritation, can contribute to maintaining a healthy genital environment.
- Regular Health Screenings: For individuals at a higher risk of sexually transmitted infections, regular health screenings and check-ups are crucial. This includes routine testing for chancroid and other infections.
- Community Outreach and Education: Community outreach programs and educational campaigns play a role in raising awareness about sexually transmitted infections, promoting safe sex practices, and encouraging individuals to seek healthcare when needed.
- Treatment of Sexual Partners: If an individual is diagnosed with chancroid, it is important that their sexual partners also seek testing and treatment to prevent the spread of the infection.
- Medical Advice and Counseling: Seeking medical advice and counseling on sexual health matters is recommended for individuals who have concerns or questions about preventing sexually transmitted infections.
Preventive measures should be tailored to individual circumstances, and individuals are encouraged to consult with healthcare providers for personalized advice based on their sexual health history and risk factors. Practicing a combination of these preventive strategies contributes to maintaining overall sexual health and reducing the risk of chancroid and other sexually transmitted infections.
What Is Herpes?
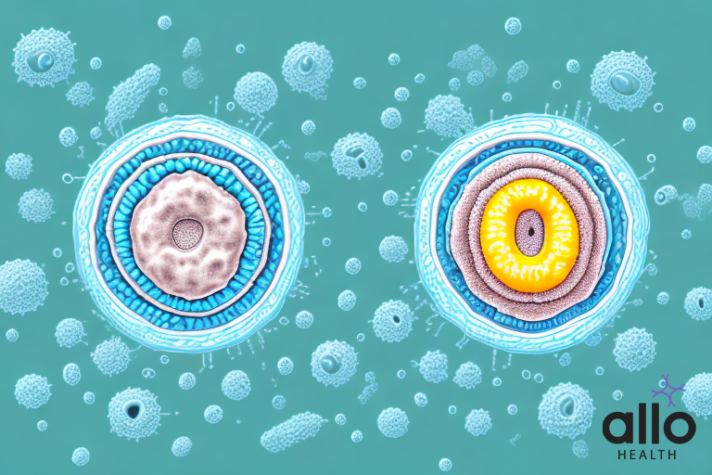
Herpes refers to a group of viral infections caused by the herpes simplex virus (HSV). There are two main types of herpes simplex virus: HSV-1 and HSV-2. While both viruses can cause oral and genital herpes infections, they are typically associated with different regions of the body. Here are the key details about herpes:
Herpes Simplex Virus Types:
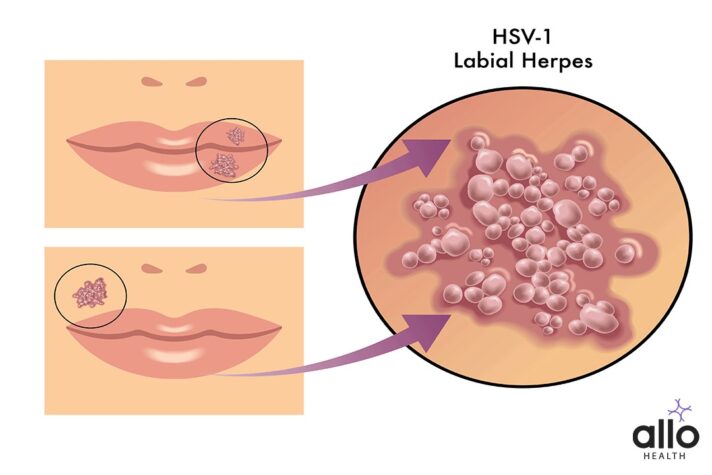
- HSV-1 (Herpes Simplex Virus Type 1):
- Often associated with oral herpes, which manifests as cold sores or fever blisters around the mouth and on the face.
- Can also cause genital herpes through oral-genital contact.
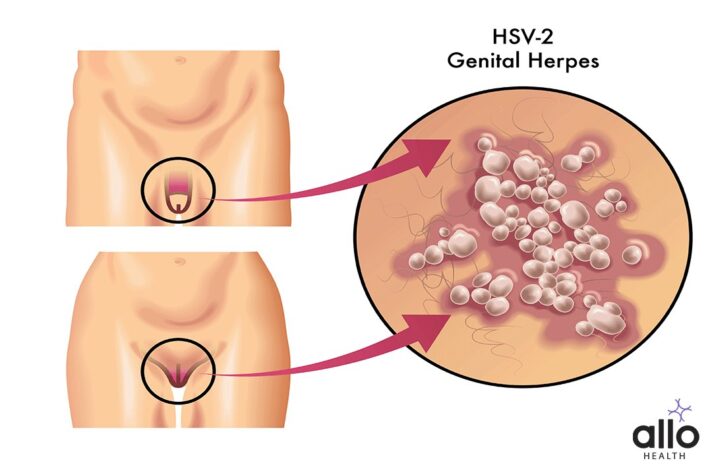
- HSV-2 (Herpes Simplex Virus Type 2):
- Mainly responsible for genital herpes, characterized by painful sores and blisters in the genital and anal areas.
- Can also cause oral herpes through genital-oral contact.
Transmission:
- Herpes is primarily transmitted through direct contact with infected skin or mucous membranes during periods of viral shedding.
- Transmission can occur through kissing, oral-genital contact, vaginal or anal intercourse, and, less commonly, through contact with genital or oral secretions.
Symptoms:
- Oral Herpes (HSV-1):
- Cold sores or fever blisters on or around the mouth.
- Itching, tingling, or burning sensations before the appearance of sores.
- Genital Herpes (HSV-2):
- Painful sores or ulcers in the genital or anal area.
- Flu-like symptoms, such as fever, headache, and swollen lymph nodes, may accompany the first outbreak.
- Asymptomatic Shedding:
- Many individuals with herpes may not exhibit noticeable symptoms but can still shed the virus and potentially transmit it to others.
Recurrent Outbreaks:
- Herpes infections are characterized by recurrent outbreaks.
- Outbreaks may be triggered by factors such as stress, illness, menstruation, or certain medications.
Diagnosis:
- Diagnosis is often based on clinical symptoms and confirmed through laboratory tests.
- Tests may include viral cultures, polymerase chain reaction (PCR) tests, and blood tests to detect antibodies to the virus.
Complications:
- While herpes is generally not life-threatening, it can cause emotional distress and may be associated with complications, particularly in individuals with weakened immune systems.
- In pregnant women, herpes can pose risks to the baby during childbirth.
Herpes and HIV:
- Herpes infection can increase the risk of acquiring or transmitting HIV.
- Individuals with herpes and HIV may experience more severe outbreaks.
Psychosocial Impact:
- Living with herpes can have emotional and psychological impacts, including stigma and concerns about disclosure.
It’s important for individuals with herpes to work closely with healthcare providers for proper management and to adopt preventive measures to reduce the risk of transmission. Education and open communication about sexual health can contribute to a better understanding of herpes and its prevention.
Herpes Symptoms And Causes
Symptoms of Herpes:
- Oral Herpes (HSV-1):
- Cold Sores or Fever Blisters:
- Small, fluid-filled blisters or sores typically appear on or around the lips.
- These sores can be painful and may be preceded by itching, tingling, or burning sensations.
- Cold sores can also occur inside the mouth or on the gums.
- Cold Sores or Fever Blisters:
- Genital Herpes (HSV-2):
- Painful Sores or Ulcers:
- Small, red bumps develop into painful sores or ulcers in the genital or anal area.
- The sores can cause discomfort, pain, and itching.
- In women, the sores may also occur on the cervix.
- Painful Sores or Ulcers:
- Flu-like Symptoms:
- During the initial outbreak, individuals may experience flu-like symptoms, including fever, headache, muscle aches, and swollen lymph nodes.
- Recurrences:
- Herpes infections are characterized by recurrent outbreaks.
- Subsequent outbreaks may have milder symptoms, shorter duration, or go unnoticed.
- Asymptomatic Shedding:
- Many individuals infected with herpes may not experience noticeable symptoms but can still shed the virus and potentially transmit it to others.
Causes of Herpes:
- Herpes Simplex Virus (HSV):
- Herpes is caused by the herpes simplex virus, with two main types:
- HSV-1 (Herpes Simplex Virus Type 1): Often associated with oral herpes.
- HSV-2 (Herpes Simplex Virus Type 2): Mainly responsible for genital herpes.
- Herpes is caused by the herpes simplex virus, with two main types:
- Transmission:
- Herpes is primarily transmitted through direct contact with infected skin or mucous membranes during periods of viral shedding.
- Common modes of transmission include kissing, oral-genital contact, vaginal or anal intercourse, and, less commonly, through contact with genital or oral secretions.
- Viral Shedding:
- Even in the absence of visible symptoms, individuals infected with herpes can shed the virus and potentially transmit it to others.
- Asymptomatic shedding can occur intermittently.
- Vertical Transmission:
- Pregnant women with genital herpes can transmit the virus to their newborn during childbirth.
- In some cases, this can lead to severe complications in the newborn.
- Risk Factors:
- Certain factors may increase the risk of acquiring or transmitting herpes, including:
- Unprotected sexual activity.
- Having multiple sexual partners.
- Having a weakened immune system.
- Previous history of other sexually transmitted infections.
- Certain factors may increase the risk of acquiring or transmitting herpes, including:
- Stress and Triggers:
- Outbreaks of herpes may be triggered by factors such as stress, illness, menstruation, or certain medications.
Herpes is a lifelong infection, and while there is no cure, proper management and preventive measures can help individuals lead healthy lives and reduce the risk of transmission to others. Regular follow-ups with healthcare providers are important for ongoing care and support.
Herpes Treatments
The treatment of herpes involves managing symptoms, reducing the frequency and severity of outbreaks, and minimizing the risk of transmission. While there is no cure for herpes, antiviral medications are commonly prescribed to achieve these goals. Here are the details of herpes treatments:
Antiviral Medications:
- Acyclovir:
- Acyclovir is one of the earliest antiviral drugs used to treat herpes.
- It is available in oral, topical, and intravenous (IV) forms.
- Common oral formulations include acyclovir tablets and capsules.
- Valacyclovir:
- Valacyclovir is a prodrug of acyclovir, meaning it is converted into acyclovir in the body.
- It is often preferred for its higher bioavailability, allowing less frequent dosing.
- Valacyclovir is typically taken orally.
- Famciclovir:
- Famciclovir is another antiviral medication used to treat herpes infections.
- It is converted into penciclovir, an active antiviral agent, in the body.
- Famciclovir is taken orally.
Treatment Goals:
- Symptom Relief: Antiviral medications can help relieve symptoms during active outbreaks, reducing pain, itching, and the duration of sores.
- Suppressive Therapy:
- For individuals with frequent or severe outbreaks, healthcare providers may recommend suppressive therapy.
- Suppressing the virus with daily antiviral medication can reduce the frequency of outbreaks and the risk of transmission.
- Reducing Viral Shedding: Antiviral drugs also help reduce viral shedding, lowering the likelihood of transmitting the virus to sexual partners.
- Shortening Outbreak Duration: Early initiation of antiviral treatment during an outbreak can shorten the duration of symptoms.
Dosage and Administration:
- Oral Medications:
- Most antiviral medications for herpes are taken orally.
- Dosage and duration of treatment depend on factors such as the specific medication, the severity of symptoms, and whether it is an initial or recurrent outbreak.
- Topical Medications:
- Some topical antiviral medications, such as topical acyclovir or penciclovir cream, may be prescribed for oral herpes lesions.
- Topical medications are less commonly used for genital herpes.
- Intravenous (IV) Medications: Intravenous acyclovir may be used in severe cases, especially in individuals with compromised immune systems.
Considerations and Side Effects:
- Timing of Treatment:
- Antiviral medications are most effective when initiated early during an outbreak.
- Starting treatment during the prodromal phase (before the appearance of sores) may provide the greatest benefit.
- Side Effects:
- Side effects of antiviral medications are generally mild and may include nausea, headache, and dizziness.
- Serious side effects are rare but can include kidney concerns (especially with high-dose IV acyclovir).
- Pregnancy and Breastfeeding:
- Pregnant women with herpes may be prescribed antiviral medications to reduce the risk of transmission to the baby during childbirth.
- Antiviral medications are generally considered safe during breastfeeding.
Herpes Prevention
Preventing herpes involves a combination of safe sex practices, antiviral medications, and lifestyle choices to reduce the risk of acquiring or transmitting the virus. Here are detailed preventive measures for herpes:
Safe Sex Practices:
- Condom Use:
- Consistent and correct use of latex or polyurethane condoms can significantly reduce the risk of genital herpes transmission.
- Condoms act as a barrier, preventing direct skin-to-skin contact and the exchange of bodily fluids.
- Dental Dams: For oral-genital contact, the use of dental dams can provide a barrier and reduce the risk of transmission.
- Communication with Partners:
- Open communication with sexual partners about sexual health, history, and concerns is crucial.
- Discussing safe sex practices and potential risks helps in making informed decisions together.
Antiviral Medications:
- Suppressive Therapy:
- Individuals with frequent or severe outbreaks may consider suppressive therapy.
- Taking antiviral medications daily can reduce the frequency of outbreaks and the risk of transmission.
- Episodic Treatment: Antiviral medications taken at the onset of symptoms during an outbreak can help shorten the duration and reduce the severity of symptoms.
- Partner Treatment: If one partner has herpes and the other does not, the infected partner taking antiviral medication can further reduce the risk of transmission.
Avoiding Contact During Outbreaks:
- Individuals with active outbreaks should avoid sexual contact, including oral-genital contact, and direct contact with oral or genital sores.
- The risk of transmission is highest during outbreaks.
Education and Awareness:
- Understanding herpes, its symptoms, and how it is transmitted is essential for prevention.
- Education helps individuals make informed decisions about sexual health and reduces the stigma associated with herpes.
Regular Health Check-ups:
- Routine check-ups with healthcare providers for sexual health screenings are crucial.
- Regular testing and monitoring help detect and manage infections early.
Avoiding High-Risk Behaviors:
- Limiting the number of sexual partners and avoiding high-risk sexual behaviors, such as unprotected sex with unknown partners, can reduce the risk of acquiring herpes.
Pregnancy Considerations:
- Pregnant women with herpes should inform their healthcare providers to manage the risk of transmission to the baby during childbirth.
- Discussing options and preventive measures during pregnancy is important.
Understanding Asymptomatic Shedding:
- Recognizing that herpes can be transmitted even when no visible symptoms are present is important.
- Taking preventive measures, including using condoms and antiviral medications, is crucial, especially when asymptomatic shedding occurs.
Psychosocial Support:
- Coping with a herpes diagnosis involves addressing emotional and psychological aspects.
- Seeking psychosocial support, such as counseling or support groups, can be beneficial.
Vaccination:
- Research is ongoing for the development of a herpes vaccine.
- Staying informed about potential advancements in vaccine research is important.
Personal Hygiene:
- Avoid sharing personal items, such as towels or razors, to prevent indirect transmission of the virus.
Disclosing Herpes Status:
- Openly disclosing one’s herpes status to sexual partners allows for informed decision-making and mutual consent.
Avoiding Irritants:
- Practices such as avoiding irritants, including certain personal hygiene products or substances that may exacerbate genital irritation, can contribute to maintaining a healthy genital environment.
Community Education:
- Community outreach programs and educational campaigns can play a role in raising awareness about herpes, promoting safe sex practices, and reducing stigma.
Preventive measures should be personalized based on individual circumstances, and individuals are encouraged to consult with healthcare providers for guidance on their specific situation. A combination of these strategies contributes to maintaining overall sexual health and reducing the risk of herpes transmission.
Comparing Chancroid and Herpes: What Are the Differences?
| Characteristic | Chancroid | Herpes |
|---|---|---|
| Causative Agent | Bacterium: Haemophilus ducreyi | Virus: Herpes Simplex Virus (HSV) |
| Transmission | Sexual contact, including vaginal, anal, and oral sex | Sexual contact, including vaginal, anal, and oral sex |
| Types of Virus | N/A (Bacterial infection) | HSV-1 (Oral herpes) and HSV-2 (Genital herpes) |
| Incubation Period | 3 to 10 days after exposure to the bacterium | Variable; typically 2 to 12 days after exposure |
| Symptoms | Painful genital ulcers, painful urination, swollen lymph nodes | Genital or oral sores, flu-like symptoms, itching, tingling |
| Ulcers Characteristics | Soft, shallow, with a sharply defined border | Painful, fluid-filled blisters or ulcers with red base |
| Purulent Discharge | Common | Less common |
| Location of Sores | Genital area primarily, may also occur in the anal region | Genital area (HSV-2) or oral/facial region (HSV-1) |
| Complications | Abscess formation, scarring | Increased risk of acquiring/transmitting other STIs, complications in pregnancy (e.g., neonatal herpes) |
| Treatment | Antibiotics (e.g., azithromycin, ceftriaxone) | Antiviral medications (e.g., acyclovir, valacyclovir) |
| Preventive Measures | Safe sex practices (condom use), partner notification | Safe sex practices (condom use), antiviral medications, education and communication |
| Vaccine Availability | No vaccine currently available | No vaccine currently available |
| Recurrence | Recurrent outbreaks common | Recurrent outbreaks common; asymptomatic shedding may occur |
| Viral Shedding | N/A (Bacterial infection) | Common, even in the absence of visible symptoms |
| Pregnancy Considerations | Chancroid does not have specific implications for pregnancy | Herpes may pose risks to the baby during childbirth; management during pregnancy is important |
| Geographic Prevalence | More common in certain regions (e.g., sub-Saharan Africa, parts of Asia) | Worldwide; prevalence varies by region |
Key Differences:
- Causative Agent:
- Chancroid is caused by a bacterium, Haemophilus ducreyi.
- Herpes is caused by the Herpes Simplex Virus (HSV-1 and HSV-2).
- Ulcer Characteristics:
- Chancroid ulcers are soft, shallow, and have a sharply defined border.
- Herpes sores are painful, fluid-filled blisters or ulcers with a red base.
- Purulent Discharge:
- Purulent discharge is common in chancroid.
- Purulent discharge is less common in herpes.
- Location of Sores:
- Chancroid primarily affects the genital area and may occur in the anal region.
- Herpes can affect the genital area (HSV-2) or the oral/facial region (HSV-1).
- Complications:
- Chancroid complications include abscess formation and scarring.
- Herpes is associated with an increased risk of acquiring/transmitting other sexually transmitted infections and complications in pregnancy.
- Treatment:
- Chancroid is treated with antibiotics (e.g., azithromycin, ceftriaxone).
- Herpes is managed with antiviral medications (e.g., acyclovir, valacyclovir).
- Vaccine Availability:
- There is currently no vaccine available for chancroid.
- There is no widely available vaccine for herpes.
- Geographic Prevalence:
- Chancroid is more common in specific regions (sub-Saharan Africa, parts of Asia).
- Herpes is a global infection with varying prevalence by region.
Key Similarities:
- Transmission: Both chancroid and herpes are primarily transmitted through sexual contact, including vaginal, anal, and oral sex.
- Symptoms: Both infections can cause painful genital sores and may lead to discomfort during urination.
- Recurrence: Both chancroid and herpes are characterized by recurrent outbreaks, and subsequent outbreaks may be milder.
- Preventive Measures:
- Safe sex practices, including condom use, are recommended for both infections.
- Antiviral medications may be used for suppressive therapy in both chancroid and herpes.
- Viral Shedding: Asymptomatic shedding of the respective pathogens can occur, allowing for transmission even in the absence of visible symptoms.
It’s crucial to consult with healthcare professionals for accurate diagnosis, appropriate treatment, and personalized prevention strategies based on individual circumstances.
Most Asked Questions
-
What is the main difference between chancroid and herpes?
Chancroid and herpes differ in their causative agents. Chancroid is caused by the bacterium Haemophilus ducreyi, while herpes is caused by the Herpes Simplex Virus (HSV-1 or HSV-2). Chancroid leads to painful genital ulcers with distinct borders, while herpes results in fluid-filled blisters or ulcers, typically in the genital or oral regions.
-
How do the symptoms of chancroid and herpes vary?
Chancroid symptoms include painful genital ulcers, painful urination, and swollen lymph nodes. In contrast, herpes manifests as genital or oral sores, flu-like symptoms, and itching or tingling sensations. Chancroid ulcers are shallow with a sharply defined border, while herpes sores are painful with a red base.
-
What are the similarities in the transmission of chancroid and herpes?
Both chancroid and herpes are primarily transmitted through sexual contact, including vaginal, anal, and oral sex. The risk of transmission is higher during active outbreaks when symptoms are present. Additionally, both infections can be spread through asymptomatic shedding, emphasizing the importance of safe sex practices.
-
How are chancroid and herpes treated, and are there specific medications?
Chancroid is treated with antibiotics like azithromycin or ceftriaxone to eliminate the bacterial infection. On the other hand, antiviral medications such as acyclovir or valacyclovir are commonly used to manage herpes symptoms, reduce the frequency of outbreaks, and lower the risk of transmission.
-
Is there a vaccine available for chancroid or herpes?
Currently, there is no widely available vaccine for either chancroid or herpes. Research is ongoing, particularly for herpes vaccines, but as of now, prevention primarily focuses on safe sex practices, antiviral medications, and awareness to minimize the risk of transmission.






































