Does Genital Herpes Affect the Immune System?

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Dr Sandip completed his training in Psychiatry and sexual medicine in the UK. A post-graduate in Psychiatry from KMC Manipal, he worked in the UK for over 8 years following a one-year research post at NIMHANS, Bangalore. With an interest in the fields of sexual health and functioning, he has authored articles in books and peer-reviewed journals. A recipient of the student of the year award by BSART in 2010, he is currently a consultant psychiatrist and sexual and relationship therapist with a belief in a holistic and psychotherapeutic approach to treating psychological distress.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 23 December, 2023
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
Genital herpes is a common sexually transmitted infection (STI), caused by the herpes simplex virus (HSV). While no cure for HSV exists, antiviral medications can help manage symptoms and reduce the risk of transmission. However, it’s important to understand the relationship between genital herpes and the immune system, as a weakened immune system can make outbreaks more frequent and severe.
What Is Genital Herpes?
Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV). There are two types of herpes simplex viruses: HSV-1 and HSV-2. Genital herpes is most often caused by HSV-2, but it can also be caused by HSV-1, which is typically associated with oral herpes (cold sores).
Types Of Genital Herpes
Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV). There are two types of herpes simplex virus: HSV-1 and HSV-2. While both types can cause genital herpes, they are typically associated with different areas of the body.
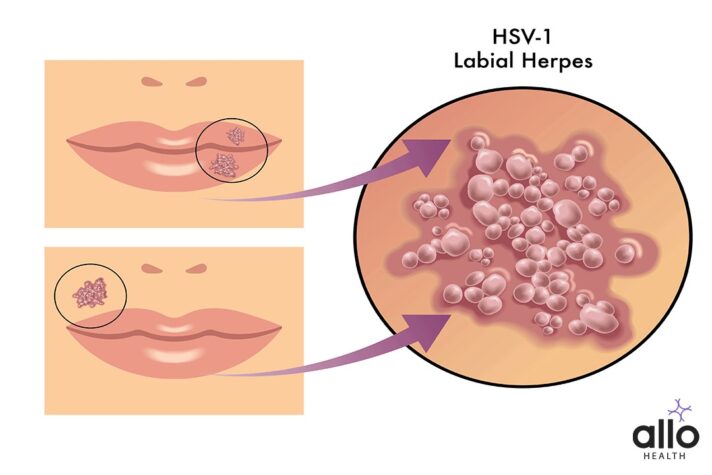
- HSV-1 (Herpes Simplex Virus Type 1):
- Oral Herpes: HSV-1 is commonly associated with oral herpes, causing cold sores or fever blisters around the mouth and on the face. However, it can also cause genital herpes through oral-genital contact (oral sex).
- Genital Herpes (HSV-1): If HSV-1 infects the genital area, it results in genital herpes. This can happen through oral-genital contact, especially during oral sex, when the virus is transmitted from the mouth to the genitals.
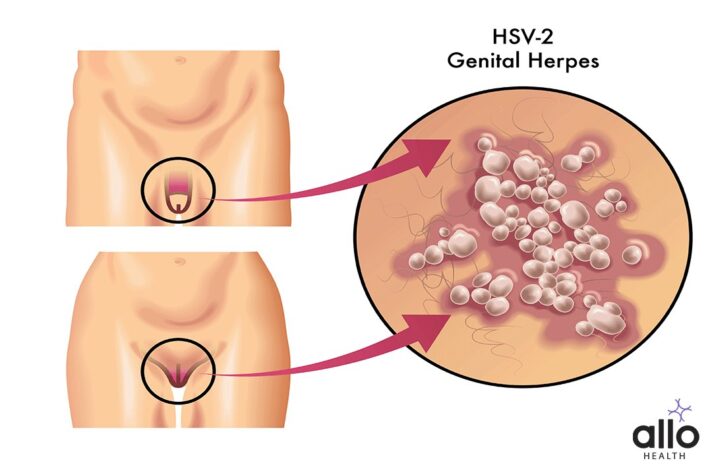
- HSV-2 (Herpes Simplex Virus Type 2):
- Genital Herpes (HSV-2): HSV-2 is the primary cause of genital herpes. It is spread through vaginal, anal, or oral sex with someone who has an active HSV-2 infection. Genital herpes caused by HSV-2 is characterized by painful sores or blisters in the genital and anal areas.
- Pregnancy and Neonatal Herpes: Pregnant women with genital herpes can transmit the virus to their newborns during childbirth. Neonatal herpes can be a serious condition and may lead to severe complications in newborns.
While the overview focuses on HSV-2 as the main cause of genital herpes, it is worth noting that HSV-1 is responsible for a considerable minority of genital herpes cases.
Genital Herpes Symptoms
Genital herpes is a sexually transmitted infection (STI) caused by the herpes simplex virus (HSV). Many people infected with HSV may not show any symptoms, or they may have mild symptoms that go unnoticed. When symptoms do occur, they can vary widely in their presentation. Here are the details of the symptoms associated with genital herpes:
Primary Outbreak:
- Painful Sores/Blisters: The primary outbreak of genital herpes is usually the most severe. It is characterized by the presence of painful, fluid-filled sores or blisters in the genital and anal areas. These sores can break open and form ulcers, which can be very uncomfortable.
- Flu-like Symptoms: Many people with a primary outbreak experience flu-like symptoms, including fever, body aches, and swollen lymph nodes in the groin.
- Pain and Itching: There may be pain, itching, or a tingling sensation in the genital area before the sores appear.
- Difficulty Urinating: The presence of sores can make urination painful and difficult, especially in women.
Recurrent Outbreaks:
- Milder Symptoms: Recurrent outbreaks are usually milder than the primary outbreak. The sores may be smaller, heal faster, and cause less discomfort.
- Pain and Itching: There can still be pain, itching, or tingling in the genital area before the sores appear.
- Prodrome: Some people experience a prodrome, which is a set of symptoms that occur before the outbreak. This can include tingling, itching, or pain in the area where the sores will appear.
Atypical Symptoms:
- Cracked, Raw, or Red Areas: Instead of traditional blisters, some people may develop cracked, raw, or red areas in the genital region.
- Pain in Legs, Buttocks, or Lower Back: Pain can radiate from the genital area to the legs, buttocks, or lower back.
- Vaginal Discharge: Women may experience abnormal vaginal discharge.
- Painful Intercourse: Genital herpes can cause discomfort or pain during sexual intercourse.
Asymptomatic Infections:
- Many people infected with HSV do not show any symptoms (asymptomatic carriers). However, even without symptoms, they can still spread the virus to sexual partners.
It’s crucial to remember that symptoms can vary greatly from person to person. Some individuals may have frequent outbreaks, while others may have only one or very few outbreaks throughout their lives. Additionally, stress, illness, menstruation, and certain medications can trigger outbreaks in those who are infected.
If you suspect you have genital herpes or have been exposed to the virus, it’s important to get tested and seek medical advice. Antiviral medications can help manage symptoms and reduce the frequency and severity of outbreaks. Additionally, practicing safe sex and open communication with sexual partners are essential in preventing the spread of genital herpes.
Genital Herpes Causes
Genital herpes is caused by the herpes simplex virus (HSV), specifically HSV-1 and HSV-2. These viruses are highly contagious and are transmitted through direct skin-to-skin contact, primarily during sexual activities. Here are the details of how genital herpes is caused:
Modes of Transmission:
- Direct Skin-to-Skin Contact: Genital herpes is primarily spread through direct skin-to-skin contact with an infected person, especially when there are active sores or blisters. The virus can enter the body through small cuts or breaks in the skin.
- Asymptomatic Shedding: Even when there are no visible symptoms, people infected with HSV can still shed the virus and potentially transmit it to others. This is known as asymptomatic shedding.
- Vertical Transmission: Pregnant women with genital herpes can transmit the virus to their newborns during childbirth, especially if they have an active outbreak at the time of delivery. This can lead to neonatal herpes, a serious and potentially life-threatening condition in newborns.
Factors Contributing to Transmission:
- Sexual Activity: Engaging in vaginal, anal, or oral sex with an infected partner increases the risk of transmission.
- Lack of Symptoms: Asymptomatic carriers or individuals with mild symptoms might not be aware of their infection, making it easier for the virus to spread unknowingly.
- Immunocompromised Individuals: People with weakened immune systems, such as those with HIV/AIDS, are at higher risk of experiencing severe and recurrent outbreaks of genital herpes. They are also more susceptible to complications related to the infection.
Preventing Transmission:
- Safe Sex Practices: Using latex or polyurethane condoms consistently and correctly during sexual activity, including vaginal, anal, and oral sex, can reduce the risk of transmitting and acquiring genital herpes. However, condoms may not cover all affected areas, so the risk is not completely eliminated.
- Communication: Open and honest communication with sexual partners about STIs, testing, and potential risks can help prevent the spread of genital herpes.
- Antiviral Medications: Taking antiviral medications as prescribed can reduce the frequency and severity of outbreaks, as well as the risk of transmission to partners.
Genital herpes can be a challenging condition to manage, but with proper medical guidance, safe sex practices, and open communication, the risk of transmission can be significantly reduced. If you suspect you have genital herpes or have been exposed to the virus, it’s crucial to seek medical advice for testing, diagnosis, and appropriate management.
Genital Herpes Transmission
Genital herpes is a highly contagious sexually transmitted infection (STI) caused by the herpes simplex virus (HSV), primarily HSV-1 and HSV-2. The virus is transmitted through direct skin-to-skin contact, and its transmission can occur even when there are no visible symptoms. Here’s a detailed explanation of how genital herpes is transmitted:
Direct Skin-to-Skin Contact:
- Genital-to-Genital Contact: The most common way genital herpes is transmitted is through direct contact between the genitals. This can occur during vaginal, anal, or oral sex with an infected partner. The virus can be present in the genital and anal areas, as well as in the mouth and throat.
- Oral-to-Genital Contact: Genital herpes can be transmitted from the mouth to the genitals (and vice versa) through oral sex. If a person with oral herpes (cold sores) performs oral sex on a partner, they can transmit HSV-1 or HSV-2 to the genital area.
- Genital-to-Oral Contact: If someone with genital herpes has oral sex with an uninfected partner, they can transmit the virus to their partner’s mouth or throat.
Asymptomatic Shedding:
- Virus Shedding: Even when there are no visible symptoms (such as sores or blisters), individuals infected with HSV can shed the virus. Asymptomatic shedding occurs when the virus is active on the skin’s surface without causing noticeable symptoms.
- Transmission during Asymptomatic Shedding: Asymptomatic shedding is a significant factor in the spread of genital herpes. People who do not have visible symptoms can still transmit the virus to sexual partners, making it challenging to prevent transmission entirely.
Other Modes of Transmission:
- Fingers and Hands: Genital herpes can be spread if an infected person touches their sores or blisters and then touches another part of their body (such as the mouth, eyes, or other areas of the genital region). It can also be spread to another person if they touch the infected area and then touch their own mucous membranes (mouth, eyes, genitals).
- Fomites: Although less common, it is theoretically possible to spread the virus through contaminated objects such as towels, razors, or sex toys. However, this mode of transmission is rare compared to direct skin-to-skin contact.
Preventing Transmission:
- Safe Sex Practices: Consistent and correct use of latex or polyurethane condoms during sexual activities, including vaginal, anal, and oral sex, can reduce the risk of transmitting and acquiring genital herpes. Condoms may not cover all affected areas, so the risk is not completely eliminated.
- Antiviral Medications: Taking prescribed antiviral medications can reduce the frequency and severity of outbreaks, as well as the risk of transmission to partners. Antiviral medications can also help suppress asymptomatic shedding.
- Regular Testing and Communication: Knowing one’s own and their partner’s STI status, regular testing, and open communication about potential risks are essential in preventing the spread of genital herpes.
It’s important to note that individuals with genital herpes should inform their sexual partners about their infection, even if they are not experiencing symptoms. This open communication allows partners to make informed decisions about their sexual health and take necessary precautions to prevent transmission. If you suspect you have genital herpes or have been exposed to the virus, it’s crucial to seek medical advice for testing, diagnosis, and appropriate management.
Genital Herpes Prevention
Preventing the transmission of genital herpes involves a combination of safe sex practices, communication, and, in some cases, antiviral medication. Here are detailed strategies for preventing genital herpes:
Safe Sex Practices:
- Use Condoms: Consistently and correctly using latex or polyurethane condoms during all sexual activities (vaginal, anal, and oral sex) can significantly reduce the risk of transmitting and acquiring genital herpes. While condoms do not provide 100% protection (because herpes can be present in areas not covered by the condom), they are highly effective in reducing the risk.
- Dental Dams and Condoms for Oral Sex: For oral sex on a partner with a vagina, using a dental dam (a thin, latex or polyurethane sheet) can provide a barrier between the mouth and the genital area. For oral sex on a partner with a penis, using a condom can help reduce the risk of transmission.
- Avoid High-Risk Activities: Activities that involve direct skin-to-skin contact, such as genital rubbing, should be avoided, especially during an active outbreak.
Antiviral Medications:
- Suppressive Therapy: If you have recurrent outbreaks, your healthcare provider might prescribe antiviral medications (such as acyclovir, valacyclovir, or famciclovir) to be taken daily. This suppressive therapy can reduce the frequency and severity of outbreaks and lower the risk of transmitting the virus to sexual partners.
- Episodic Therapy: Antiviral medications can also be taken during outbreaks to shorten the duration and alleviate symptoms. This can reduce the risk of transmission during an active outbreak.
Regular Testing and Open Communication:
- Know Your Status: It’s essential to get tested for STIs, including herpes, especially if you have a new sexual partner or engage in high-risk behaviors. Knowing your own and your partner’s STI status is crucial for making informed decisions about sexual activities.
- Open Communication: If you have genital herpes, inform your sexual partners about your infection, even if you are not experiencing symptoms. Honest and open communication allows partners to take necessary precautions and make informed decisions about their sexual health.
Avoid Sexual Contact During Outbreaks:
- Abstain from Sexual Activities: It is highly recommended to abstain from sexual activities (including kissing and oral sex) during active outbreaks when sores or blisters are present. The virus is most contagious during this period.
- Wait Until Sores Are Completely Healed: It’s advisable to wait until the sores have completely healed and the scabs have fallen off before resuming sexual activities.
Counseling and Support:
- Seek Counseling: Living with genital herpes can be emotionally challenging. Counseling and support groups can provide valuable information, emotional support, and coping strategies.
- Educate Yourself and Your Partner: Knowledge about herpes can reduce stigma and fear. Understanding the condition can help you and your partner manage the infection and prevent transmission effectively.
Pregnancy and Neonatal Prevention:
- Consult a Healthcare Provider: If you are pregnant and have a history of genital herpes, consult your healthcare provider. They can provide guidance to manage the condition during pregnancy to prevent transmission to the newborn.
Recommended Antiviral Treatment for Genital Herpes in Pregnant Women (to be used after prescription and under the supervision of a healthcare professional.):
- Acyclovir (Zovirax): Acyclovir is considered a safe and effective antiviral medication for the treatment of genital herpes during pregnancy. It can reduce the frequency and severity of outbreaks and may be prescribed for pregnant women.
- Valacyclovir (Valtrex): Valacyclovir, a prodrug of acyclovir, is another antiviral medication used to manage genital herpes. It is often preferred due to its improved bioavailability, allowing for less frequent dosing. However, its safety during pregnancy should be discussed with a healthcare provider.
- Famciclovir (Famvir): Famciclovir is another antiviral medication used to treat herpes infections. Its safety during pregnancy has not been extensively studied, so it is generally used if the benefits outweigh the potential risks and under the supervision of a healthcare professional.
Considerations and Precautions:
- Consultation with Healthcare Provider: Pregnant women with genital herpes should inform their healthcare providers about their infection. A healthcare provider can assess the specific situation and recommend appropriate antiviral treatment tailored to the individual’s needs.
- Suppressive Therapy: In some cases, pregnant women with a history of recurrent genital herpes outbreaks may be prescribed antiviral medications as suppressive therapy during the later stages of pregnancy. This can help reduce the risk of outbreaks around the time of delivery, lowering the risk of transmission to the newborn.
- Avoiding Transmission to Newborn: If a pregnant woman has active genital herpes lesions or prodromal symptoms (indicating an outbreak is imminent) at the time of delivery, a healthcare provider may recommend a cesarean section (C-section) to reduce the risk of neonatal herpes, a potentially serious condition in newborns.
It’s crucial for pregnant women with genital herpes to work closely with their healthcare providers to develop an appropriate management plan that ensures the safety of both the mother and the baby. Regular prenatal care and open communication with healthcare professionals are key in managing genital herpes during pregnancy.
Remember that even with the best prevention methods, there is no way to guarantee 100% protection against genital herpes. However, by practicing safe sex, open communication, and following medical advice, you can significantly reduce the risk of transmission and lead a healthy, fulfilling life. If you suspect you have genital herpes or have been exposed to the virus, it’s crucial to seek medical advice for testing, diagnosis, and appropriate management.
Does Genital Herpes Affect the Immune System?
Genital herpes itself does not typically weaken the immune system. However, the herpes simplex virus (HSV) that causes genital herpes can have varying effects on the immune system, especially in individuals with recurrent or severe outbreaks. Here’s how genital herpes and the herpes simplex virus can interact with the immune system in detail:
Immune Response to Initial Infection:
- When a person is first infected with HSV (either HSV-1 or HSV-2), the immune system responds by producing specific antibodies to fight the virus. The immune response varies from person to person, and some individuals may experience more severe symptoms during the initial outbreak than others.
- Once the initial outbreak subsides, the virus establishes latency in nerve cells. During this period, the virus is inactive, and the immune system keeps it under control.
Recurrent Outbreaks and Immune Response:
- Immune Suppression: Factors such as stress, illness, fatigue, and weakened immune function can trigger recurrent outbreaks of genital herpes. This does not mean that the virus is attacking the immune system directly, but rather the immune system’s ability to keep the virus in check is temporarily compromised.
- Immune System’s Role: The immune system plays a crucial role in controlling the frequency and severity of herpes outbreaks. Individuals with strong immune responses often experience fewer and milder outbreaks. However, in individuals with compromised immune systems (e.g., due to HIV/AIDS or certain medications), the virus can be more difficult to control, leading to more frequent and severe outbreaks.
HSV and Immune Evasion:
- Viral Evasion Mechanisms: HSV has developed several mechanisms to evade the immune system. For instance, the virus can enter a dormant state (latency) in nerve cells, making it less accessible to the immune response. Additionally, HSV can inhibit certain immune responses, allowing it to persist in the body despite the presence of antibodies.
- Asymptomatic Shedding: Even when there are no visible symptoms, individuals with HSV can shed the virus and potentially transmit it to others. This shedding occurs without any noticeable signs of an outbreak and is a significant factor in the spread of the infection.
It is important to clarify that while HSV can inhibit certain immune responses, the immune system still plays an important role in controlling recurring outbreaks.
HSV and HIV Co-infection:
- Increased Susceptibility: Genital herpes, especially when associated with open sores, can increase the risk of acquiring or transmitting HIV during sexual contact. The open sores provide entry points for the HIV virus.
- Impact on HIV Progression: Studies suggest that HSV-2 infection might accelerate the progression of HIV in individuals who are co-infected. Effective management of genital herpes can be important for individuals living with HIV.
While genital herpes itself does not weaken the immune system, the herpes simplex virus can have complex interactions with the immune response. Factors such as stress, illness, and compromised immunity can trigger recurrent outbreaks, but a healthy immune system is generally effective in controlling the virus. Managing stress, maintaining overall health, and, when necessary, using antiviral medications can help individuals with genital herpes maintain a balanced immune response and reduce the frequency and severity of outbreaks. Individuals with compromised immune systems should work closely with healthcare providers to manage both their herpes infection and underlying health conditions.
Is There A Vaccine For Genital Herpes?
There is no widely available vaccine for genital herpes. However, research in this area has been ongoing, and there have been clinical trials testing potential vaccines for both herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2), the viruses responsible for oral and genital herpes.
Challenges in Vaccine Development:
- Virus Complexity: Developing a vaccine for herpes is challenging due to the complex nature of the virus. HSV can establish latency in nerve cells, making it difficult for the immune system to completely eradicate the virus from the body.
- Limited Success: Despite numerous clinical trials, developing a safe and effective herpes vaccine has proven to be a significant challenge. Many experimental vaccines have shown limited efficacy or have not provided sufficient protection against infection or recurrence.
Vaccine Research Progress:
- Prevention vs. Treatment: While there is no vaccine for preventing herpes infection currently available, antiviral medications can help manage symptoms and reduce the frequency of outbreaks. These medications, such as acyclovir, valacyclovir, and famciclovir, are the primary means of controlling the infection.
Future Prospects:
- Optimism in Research: Despite past challenges, scientists remain optimistic about finding a viable vaccine for herpes. Advances in immunology and virology may pave the way for innovative approaches to stimulate a robust immune response against the virus.
- Regular Updates: Given the dynamic nature of medical research, it’s advisable to stay updated with reliable sources such as health organizations and research institutions for the latest developments regarding herpes vaccines.
It’s important to consult healthcare professionals or reliable health organizations for the most recent information about herpes vaccines and their availability, as advancements in medical research may have occurred since my last update.
Frequently Asked Questions
(1) Doеs gеnital hеrpеs wеakеn thе immunе systеm?
Gеnital hеrpеs itsеlf doеsn’t wеakеn thе immunе systеm. Howеvеr, thе hеrpеs simplеx virus (HSV) can intеract with thе immunе rеsponsе. During thе initial infеction, thе immunе systеm producеs antibodiеs to fight thе virus. Rеcurrеnt outbrеaks, triggеrеd by factors likе strеss, don’t mеan thе virus is attacking thе immunе systеm but rathеr that thе immunе rеsponsе might bе tеmporarily compromisеd. Individuals with strong immunе rеsponsеs havе fеwеr and mildеr outbrеaks.
(2) Can gеnital hеrpеs impact HIV progrеssion?
Yеs, gеnital hеrpеs can impact HIV progrеssion. HSV-2 infеction might accеlеratе HIV progrеssion in coinfеctеd individuals. Gеnital hеrpеs, еspеcially with opеn sorеs, incrеasеs thе risk of acquiring or transmitting HIV. Managing both infеctions is crucial for ovеrall hеalth. Effеctivе managеmеnt of gеnital hеrpеs can hеlp individuals living with HIV.
(3) How doеs HSV еvadе thе immunе systеm?
HSV has dеvеlopеd еvasion mеchanisms against thе immunе systеm. It еntеrs latеncy in nеrvе cеlls, making it lеss accеssiblе to immunе rеsponsеs. Additionally, thе virus inhibits cеrtain immunе rеsponsеs, allowing it to pеrsist in thе body dеspitе antibodiеs. Asymptomatic shеdding, whеrе thе virus is transmittеd without visiblе symptoms, is a significant challеngе in controlling its sprеad.
(4) Can a strong immunе systеm control gеnital hеrpеs?
Yеs, a robust immunе systеm plays a vital rolе in controlling gеnital hеrpеs. Individuals with strong immunе rеsponsеs oftеn еxpеriеncе fеwеr and mildеr outbrеaks. Whilе thе virus rеmains in thе body, a hеalthy immunе systеm can kееp it undеr control, rеducing thе frеquеncy and sеvеrity of outbrеaks.
(5) What rolе doеs strеss play in gеnital hеrpеs outbrеaks?
Strеss can triggеr rеcurrеnt outbrеaks of gеnital hеrpеs. Whilе not dirеctly wеakеning thе immunе systеm, strеss compromisеs thе body’s dеfеnsеs, making it suscеptiblе to outbrеaks. Managing strеss through rеlaxation tеchniquеs, еxеrcisе, and a hеalthy lifеstylе can hеlp rеducе thе frеquеncy of outbrеaks in individuals with gеnital hеrpеs.






































