Understanding Endometriosis Ovulation Pain and How to Manage It

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Dr Sanina Mansoor holds MBBS degree from Yenepoya university,Mangalore.She has 8 years of experience working as a medical officer at various health centres and medical colleges.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 17 March, 2024
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
Endometriosis ovulation pain is a common symptom experienced by women with endometriosis. It can be a sharp, stabbing pain that occurs during ovulation or a dull ache that lasts for several days. In this article, we will discuss what endometriosis ovulation pain is, what causes it, and how you can manage it to improve your quality of life.
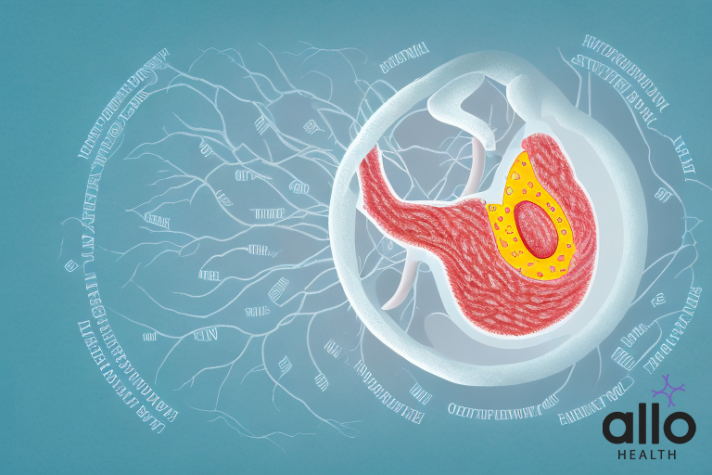
What Is Endometriosis?
Endometriosis is a medical condition that occurs when tissue similar to the lining of the uterus, called the endometrium, grows outside the uterus. Normally, the endometrium thickens, breaks down, and is shed during the menstrual cycle. However, when endometrial tissue is present outside the uterus, it cannot be easily expelled from the body. This can lead to various symptoms and complications.
Here are some key aspects of endometriosis:
- Location of Growth: Endometriosis can occur on various pelvic organs, such as the ovaries, fallopian tubes, outer surface of the uterus, and the lining of the pelvic cavity. In rare cases, it can even be found outside the pelvic region, affecting areas like the intestines or bladder.
- Formation of Endometrial Implants: The misplaced endometrial tissue can form implants or lesions. These implants respond to hormonal changes in the menstrual cycle, just like the normal endometrium inside the uterus. As a result, they may bleed, causing inflammation, pain, and the formation of scar tissue.
- Symptoms: Endometriosis is often associated with pelvic pain, which can range from mild to severe. Other common symptoms include painful menstrual cramps, pain during or after sex, irregular menstrual cycles, and gastrointestinal issues such as bloating, constipation, or diarrhea.
- Diagnosis: Diagnosis of endometriosis typically involves a combination of medical history review, pelvic examination, imaging studies (such as ultrasound), and sometimes a surgical procedure called laparoscopy. Laparoscopy allows the doctor to directly visualize and confirm the presence of endometrial implants.
- Impact on Fertility: Endometriosis can be a significant factor in infertility. The exact relationship between endometriosis and fertility is not fully understood, but it is believed that the presence of scar tissue and distorted pelvic anatomy may interfere with the normal reproductive process.
- Treatment: Treatment options for endometriosis aim to relieve symptoms, reduce the size and number of endometrial implants, and improve fertility if desired. Common approaches include pain medication, hormonal therapy (such as birth control pills or gonadotropin-releasing hormone agonists), and surgery to remove endometrial tissue.
- Lifestyle Management: Some individuals find relief from symptoms through lifestyle changes, such as maintaining a healthy diet, regular exercise, and managing stress. These measures can complement medical treatments.
Endometriosis is a chronic condition that often requires ongoing management. A multidisciplinary approach involving gynecologists, pain specialists, and fertility experts may be necessary to address the various aspects of the condition and its impact on a person’s life. If you suspect you have endometriosis or are experiencing symptoms, it’s important to consult with a healthcare professional for proper evaluation and guidance.
 What Is Ovulation?
What Is Ovulation?
Ovulation is a key event in the menstrual cycle of females, marking the release of a mature egg (ovum) from one of the ovaries. This process is essential for reproduction and occurs approximately midway through the menstrual cycle. Here is a detailed overview of ovulation:
- Menstrual Cycle Phases: The menstrual cycle is divided into several phases, with ovulation occurring in the middle of the cycle. The main phases include menstruation, the follicular phase, ovulation, and the luteal phase.
- Follicular Phase: The menstrual cycle begins with the follicular phase, during which the pituitary gland releases follicle-stimulating hormone (FSH). FSH stimulates the development of multiple follicles within the ovaries, each containing an immature egg. Only one of these follicles will become dominant and mature.
- Ovulation: As the dominant follicle matures, it releases increasing amounts of estrogen. The rising estrogen levels trigger a surge in luteinizing hormone (LH) around the middle of the menstrual cycle. This surge in LH prompts the mature follicle to release the mature egg from the ovary. This release of the egg is ovulation.
- Ovarian Release: Ovulation involves the rupture of the mature follicle, releasing the egg into the fallopian tube. The egg is then available for fertilization by sperm. The timing of ovulation is crucial for achieving pregnancy because the egg is viable for fertilization for a relatively short period—usually around 12 to 24 hours.
- Luteal Phase: After ovulation, the ruptured follicle transforms into a structure called the corpus luteum. This structure produces progesterone, a hormone that prepares the uterine lining for a potential pregnancy. If fertilization does not occur, the corpus luteum degenerates, leading to a decline in progesterone levels and the initiation of menstruation.
- Menstruation: If the egg is not fertilized and there is no pregnancy, the thickened uterine lining is shed during menstruation, and the menstrual cycle begins anew.
- Fertility and Tracking Ovulation: Ovulation is a crucial factor in fertility. Couples trying to conceive often track ovulation to identify the most fertile days of the menstrual cycle. This can be done using various methods, including tracking menstrual cycles, monitoring basal body temperature, using ovulation predictor kits, and observing changes in cervical mucus.
Understanding ovulation is important for family planning, whether a person is trying to conceive or trying to prevent pregnancy. If there are concerns about irregular ovulation or difficulties conceiving, consulting with a healthcare professional or a fertility specialist can provide valuable guidance and support.
What is Endometriosis Ovulation Pain?
Endometriosis ovulation pain refers to pelvic discomfort or pain experienced by individuals with endometriosis specifically during ovulation, the phase of the menstrual cycle when the ovary releases a mature egg. It’s important to note that not everyone with endometriosis experiences ovulation pain, and the severity of symptoms can vary among individuals.
Here are some key points about endometriosis ovulation pain:
- Association with Ovulation: Ovulation pain in the context of endometriosis occurs around the time of egg release from the ovary. This pain is often cyclic and may coincide with the midpoint of the menstrual cycle.
- Location of Pain: The pain is typically felt in the pelvic region, on one or both sides of the lower abdomen. The exact location can vary among individuals. Some may experience pain on the same side consistently, while others may alternate sides.
- Characteristics of Pain: The pain associated with endometriosis ovulation can be sharp, stabbing, or cramp-like. It may be mild or more intense, lasting from a few hours to a couple of days.
- Differentiation from Regular Ovulation Pain: While many women may experience mild discomfort or twinges during ovulation, the pain associated with endometriosis tends to be more intense and may be accompanied by other endometriosis-related symptoms.
- Possible Causes: The exact cause of ovulation pain in individuals with endometriosis is not fully understood. It is believed that the presence of endometrial tissue outside the uterus, including on the ovaries, can contribute to inflammation, causing pain during ovulation.
- Impact on Fertility: For some individuals with endometriosis, the presence of endometrial implants on the ovaries or fallopian tubes can impact fertility. Ovulation pain may be an indication of underlying issues that could affect the ability to conceive.
- Management and Treatment: Managing endometriosis ovulation pain often involves a combination of medical and lifestyle interventions. Pain relief medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may be recommended. Hormonal therapies, such as birth control pills or gonadotropin-releasing hormone agonists, may also be used to regulate the menstrual cycle and reduce symptoms.
- Consulting a Healthcare Professional: If an individual with endometriosis experiences severe or worsening ovulation pain, or if there are concerns about fertility, it is crucial to consult with a healthcare professional. A gynecologist or specialist in reproductive health can assess the specific situation, provide a proper diagnosis, and recommend appropriate management strategies.
Overall, understanding and addressing ovulation pain in the context of endometriosis require individualized care and a comprehensive approach to managing the underlying condition.
Symptoms Of Endometriosis Ovulation Pain
Endometriosis ovulation pain shares some common symptoms with general ovulation discomfort, but in the context of endometriosis, these symptoms can be more pronounced and associated with the presence of endometrial tissue outside the uterus. Here’s a detailed look at the symptoms of endometriosis ovulation pain:
- Pelvic Pain: The hallmark symptom of endometriosis ovulation pain is pelvic discomfort or pain. This pain is often localized to one side of the lower abdomen and can range from a dull ache to a sharp, stabbing sensation. The intensity may vary among individuals and can be more severe than typical ovulation pain.
- Cyclical Nature: Endometriosis ovulation pain tends to be cyclical, occurring around the time of ovulation in the middle of the menstrual cycle. This cyclic nature distinguishes it from non-cyclical pelvic pain and may help identify the association with the release of the egg from the ovary.
- Painful Intercourse: Some individuals with endometriosis experience pain during or after sexual intercourse, and this symptom may be more pronounced during ovulation. The presence of endometrial implants on the ovaries or surrounding pelvic structures can contribute to discomfort.
- Irregular Menstrual Cycles: Endometriosis can disrupt the normal hormonal regulation of the menstrual cycle. Individuals with endometriosis may experience irregular menstrual cycles, and ovulation pain may coincide with these irregularities.
- Gastrointestinal Symptoms: Endometriosis ovulation pain can be accompanied by gastrointestinal symptoms such as bloating, constipation, or diarrhea. The proximity of endometrial implants to the intestines may contribute to these symptoms during the menstrual cycle.
- Back Pain: Some individuals with endometriosis report experiencing lower back pain, which may be associated with ovulation. This pain can radiate from the pelvic region to the lower back, contributing to overall discomfort.
- Painful Bowel Movements: Endometrial implants on the rectum or bowel can lead to pain during bowel movements, especially during the menstrual cycle. This symptom may be more pronounced during ovulation.
- Fatigue and Malaise: Chronic pain associated with endometriosis ovulation may contribute to feelings of fatigue and overall malaise. The impact on daily activities and quality of life can be substantial.
It’s important to note that not everyone with endometriosis experiences ovulation pain, and the severity of symptoms can vary. If an individual suspects they have endometriosis or is experiencing significant ovulation pain, consulting with a healthcare professional is crucial for proper evaluation, diagnosis, and management.
Causes Of Endometriosis Ovulation Pain
The causes of ovulation pain in individuals with endometriosis are not fully understood, but several factors may contribute to the discomfort experienced during this phase of the menstrual cycle. Endometriosis is a condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus. Here are some potential causes of ovulation pain in the context of endometriosis:
- Presence of Endometrial Implants on the Ovaries: Endometrial tissue can implant itself on various pelvic organs, including the ovaries. This tissue responds to hormonal changes during the menstrual cycle, just like the normal endometrium inside the uterus. The presence of endometrial implants on the ovaries may contribute to inflammation and pain, particularly during ovulation.
- Adhesions and Scar Tissue: Endometriosis can lead to the formation of adhesions and scar tissue in the pelvic region. These adhesions may distort the normal anatomy of the reproductive organs, causing pain during ovulation as the ovary releases an egg and the fallopian tubes facilitate its journey to the uterus.
- Inflammation: Endometriosis is associated with chronic inflammation. Inflammation in the pelvic cavity can contribute to pain during various phases of the menstrual cycle, including ovulation. The inflammatory response may be heightened during ovulation, leading to increased discomfort.
- Stimulation of Nerve Endings: Endometriosis can stimulate nerve endings in the pelvic region, leading to heightened sensitivity and pain perception. During ovulation, the release of the egg and the associated hormonal changes may further stimulate these nerves, contributing to pain.
- Cyclical Hormonal Changes: Ovulation is a hormonal event marked by a surge in luteinizing hormone (LH) that triggers the release of the mature egg from the ovary. The hormonal fluctuations during the menstrual cycle, especially the rise and fall of estrogen and progesterone, can influence the growth and activity of endometrial tissue outside the uterus, potentially leading to pain.
- Individual Variability: The experience of ovulation pain can vary among individuals with endometriosis. Factors such as the location and extent of endometrial implants, the presence of adhesions, and the overall severity of the condition can contribute to the variability in symptoms.
It’s important to note that while ovulation pain can be a symptom of endometriosis, not all individuals with endometriosis experience this specific type of discomfort. Additionally, other conditions unrelated to endometriosis can also cause ovulation pain.
If someone is experiencing significant or worsening ovulation pain in the context of endometriosis, it is advisable to consult with a healthcare professional. A gynecologist or specialist can assess the individual’s specific situation, provide a proper diagnosis, and recommend appropriate management strategies, which may include pain relief medications, hormonal therapies, or other interventions tailored to the individual’s needs.
How To Manage Endometriosis Ovulation Pain?
Managing endometriosis ovulation pain involves a combination of medical, lifestyle, and self-care strategies. It’s important to note that the effectiveness of these approaches can vary among individuals, and a personalized plan in consultation with a healthcare professional is recommended. Here are detailed strategies for managing endometriosis ovulation pain:
- Pain Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help alleviate pain and reduce inflammation. These medications are commonly used to manage menstrual cramps and can be effective in addressing ovulation pain.
- Prescription Medications: In more severe cases, a healthcare provider may prescribe stronger pain medications. Hormonal medications, such as birth control pills, may also be recommended to regulate the menstrual cycle and reduce pain associated with endometriosis.
- Hormonal Therapies: Hormonal treatments, such as gonadotropin-releasing hormone (GnRH) agonists or progestin-only therapies, may be prescribed to suppress ovulation and the growth of endometrial tissue. These therapies can help manage pain symptoms throughout the menstrual cycle.
- Heat Therapy: Applying heat to the lower abdomen can provide relief from pelvic pain. A hot water bottle, heating pad, or warm bath can help relax muscles and ease discomfort. Heat therapy is a simple and non-invasive way to manage pain.
- Physical Activity: Regular exercise has been shown to reduce pain and improve overall well-being in individuals with endometriosis. Low-impact activities such as walking, swimming, or yoga may be beneficial. However, it’s essential to listen to the body and choose activities that are comfortable.
- Dietary Modifications: Some individuals find that certain dietary changes can help manage endometriosis symptoms. While research on the impact of diet is ongoing, some people report relief by avoiding inflammatory foods, such as processed foods, caffeine, and excessive amounts of red meat.
- Stress Management: Chronic stress can exacerbate pain symptoms. Techniques such as mindfulness, meditation, deep breathing exercises, and relaxation techniques can help manage stress levels and potentially reduce pain.
- Acupuncture and Physical Therapy: Some individuals with endometriosis find relief through alternative therapies such as acupuncture. Physical therapy, including pelvic floor physical therapy, can also be beneficial in addressing muscle tension and pain associated with endometriosis.
- Counseling and Support Groups: Living with a chronic condition like endometriosis can be emotionally challenging. Seeking support through counseling or joining support groups can provide emotional support, coping strategies, and a sense of community.
- Surgical Intervention: In cases where conservative measures are not effective, or if endometriosis is severe, surgical intervention may be considered. Laparoscopic surgery can be performed to remove endometrial implants, adhesions, and cysts, potentially providing relief from symptoms.
It’s crucial for individuals experiencing endometriosis ovulation pain to work closely with their healthcare provider to develop a comprehensive management plan tailored to their specific needs and symptoms. Regular communication with a healthcare professional allows for adjustments to the treatment plan as needed and ensures ongoing support for managing this chronic condition.
Most Asked Questions
-
What causes ovulation pain in individuals with endometriosis?
Ovulation pain in endometriosis is primarily attributed to the presence of endometrial tissue outside the uterus. This tissue, responding to hormonal changes, can lead to inflammation, adhesions, and stimulation of pelvic nerves, resulting in pain during the release of an egg.
-
How can I manage endometriosis ovulation pain at home?
Home management includes using over-the-counter NSAIDs for pain relief, applying heat to the lower abdomen, practicing regular exercise such as yoga or walking, and exploring stress-reduction techniques like meditation. Dietary modifications and alternative therapies like acupuncture may also offer relief.
-
Are there specific medications to alleviate endometriosis ovulation pain?
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can be effective in reducing pain. Hormonal therapies, including birth control pills or GnRH agonists, may be prescribed to regulate the menstrual cycle and manage pain. Prescription pain medications may also be recommended for severe cases.
-
Can endometriosis ovulation pain impact fertility?
While ovulation pain itself may not directly affect fertility, endometriosis, if left untreated, can lead to the formation of adhesions and scar tissue that may impact reproductive organs. Seeking early intervention and management can be crucial for those trying to conceive.
-
When should I seek medical advice for endometriosis ovulation pain?
Consult a healthcare professional if you experience severe or worsening ovulation pain, if pain interferes with daily activities, or if you have concerns about fertility. A gynecologist can assess your symptoms, provide a proper diagnosis, and recommend appropriate management

 What Is Ovulation?
What Is Ovulation?




































