Retrograde Ejaculation Prognosis: Insights into Prognosis and Treatment Options

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Ms Ashima Sahore has a masters in Clinical Psychology and has been working avidly in the space of therapy and research for the past 2 years. Her expertise lies in areas of stress, depression, anxiety, improving self-esteem, confidence, body appreciation among many others. She imbibes a wholesome approach to therapy and provides a non-judgemental, LGBTQAI+, and safe space.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 26 December, 2023
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
The understanding of male sexual health and reproductive disorders has grown exponentially in recent years, with advances in medical research shedding light on conditions that were once considered enigmatic. Retrograde ejaculation (RE) is one such condition.
What is Retrograde Ejaculation?
Retrograde ejaculation, also known as dry orgasm, is a condition in which semen, instead of being expelled out through the penis during ejaculation, enters the urinary bladder. Normally, during ejaculation, the muscles at the neck of the bladder close off the bladder opening, allowing semen to travel through the urethra and exit the body. However, in (RE), these muscles fail to function properly, resulting in the redirection of semen into the bladder.
The most common cause of (RE) is the dysfunction of the bladder neck muscles or the sphincter that controls the flow of urine. This dysfunction can be caused by various factors, including:
- Medical Conditions: (RE) can occur as a result of certain medical conditions such as diabetes, multiple sclerosis, spinal cord injuries, prostate surgery, or certain medications used to treat high blood pressure, prostate enlargement, or psychiatric disorders.
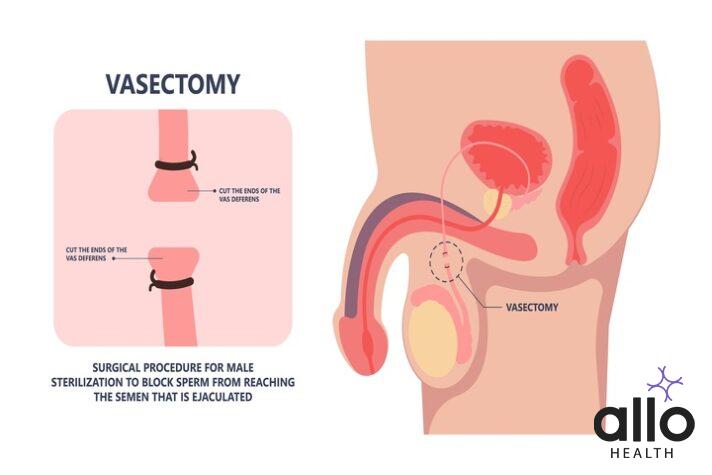
- Surgical Procedures: Certain surgical procedures, particularly those involving the prostate or the neck of the bladder, can lead to damage or disruption of the muscles responsible for closing off the bladder during ejaculation.
- Nerve Damage: Damage to the nerves that control the bladder neck muscles can impair their ability to function properly, leading to retrograde ejaculation. Nerve damage can occur due to diabetes, spinal cord injuries, or pelvic surgery.
The main symptom of retrograde ejaculation is a reduced or absence of semen during orgasm. Instead of a normal ejaculation, the semen may either be released in small amounts or not at all. Men with retrograde ejaculation may also notice cloudy urine after sexual activity, as the semen mixes with the urine in the bladder.
Retrograde ejaculation is generally not harmful or painful, but it can cause fertility concerns. Since the semen does not exit the penis, it becomes difficult for sperm to reach the cervix and fertilize an egg during intercourse. This can lead to difficulties in achieving pregnancy. However, in some cases, retrograde ejaculation may be an unintended consequence of surgical procedures performed to address fertility concerns.
Diagnosing Retrograde Ejaculation
The diagnosis of retrograde ejaculation typically involves a combination of medical history, physical examination, and specialized tests. Here is a detailed overview of the diagnostic process:
- Medical History: The healthcare professional will start by taking a detailed medical history, including questions about symptoms, their duration and severity, and any factors that may contribute to retrograde ejaculation. They may inquire about any past surgeries, medical conditions (such as diabetes or multiple sclerosis), medications being taken, or any previous fertility concerns.
- Physical Examination: A physical examination may be performed to assess the overall health and identify any physical abnormalities that could contribute to retrograde ejaculation. The healthcare professional may examine the genital area, including the penis, scrotum, and prostate, to check for any signs of structural abnormalities, surgical scars, or enlarged prostate.
- Semen Analysis: A semen analysis is usually conducted to evaluate the quantity and quality of sperm in the ejaculate. In the case of retrograde ejaculation, the semen sample will be collected immediately after ejaculation, typically by urinating into a special container, to determine if semen is entering the bladder instead of being expelled from the penis. The sample will then be examined under a microscope to assess sperm count, motility, and morphology.
- Post-Ejaculatory Urinalysis: After collecting the semen sample, a post-ejaculatory urinalysis is performed to check for the presence of sperm in the urine. If retrograde ejaculation is present, the urine sample collected after ejaculation will contain semen and sperm.
- Specialized Tests: In some cases, specialized tests may be conducted to determine the underlying cause of retrograde ejaculation. These tests may include:
- Urodynamic Testing: This test measures the pressure and flow of urine during urination to assess the bladder’s function and determine if there are any abnormalities that contribute to (RE)
- Imaging Studies: Imaging techniques, such as ultrasound or X-ray, may be used to visualize the bladder and the structures involved in ejaculation to identify any structural abnormalities or damage.
- Nerve Function Tests: Nerve conduction studies or electromyography (EMG) may be performed to evaluate the function and integrity of the nerves involved in ejaculation.
The combination of medical history, physical examination, semen analysis, and specialized tests helps healthcare professionals accurately diagnose (RE) and determine its underlying cause. This information is crucial for developing an appropriate treatment plan tailored to the individual’s needs and fertility goals. It is recommended to consult with a healthcare professional, such as a urologist or a reproductive endocrinologist, for a thorough evaluation and diagnosis.
Prognosis of Retrograde Ejaculation
The prognosis of retrograde ejaculation depends on the underlying cause and individual factors. In some cases, the condition may be temporary and reversible, while in others, it may be a chronic or permanent condition. Here are some factors that can influence the prognosis:
- Underlying Cause: If (RE) is caused by medications, such as certain alpha-blockers used to treat high blood pressure, it may resolve once the medication is discontinued or switched to an alternative. Similarly, if the condition is a result of a reversible medical condition, such as a urinary tract infection, treating the underlying cause can restore normal ejaculation.
- Surgical Procedures: If (RE) is a result of surgery, the prognosis may vary depending on the type of surgery performed and the extent of damage to the bladder neck or associated nerves. In some cases, the condition may improve over time as the body adjusts and compensates for the changes. However, in other cases, the damage may be irreversible, leading to long-term or permanent retrograde ejaculation.
- Nerve Damage: If RE is caused by nerve damage, the prognosis can be more challenging. The extent and location of the nerve damage play a significant role in determining the potential for recovery. In cases where the nerves are partially damaged but still functional, treatment options such as medications or nerve stimulation techniques may help restore ejaculation to some extent. However, if the nerves are severely damaged or completely non-functional, the prognosis for restoring normal ejaculation may be poor.
- Fertility Considerations: For men who are concerned about fertility, the prognosis of RE can have implications for their ability to conceive naturally. Since RE redirects semen into the bladder instead of expelling it through the penis, it can affect fertility by reducing or eliminating the sperm that reach the cervix during intercourse. However, assisted reproductive techniques, such as intrauterine insemination (IUI) or in vitro fertilization (IVF), can still offer opportunities for conception by bypassing the issue of retrograde ejaculation.
It’s important to note that the prognosis of retrograde ejaculation can vary from person to person, and individual responses to treatment can differ. Consulting with a healthcare professional, such as a urologist or a reproductive endocrinologist, can provide a more accurate prognosis based on the specific circumstances and underlying causes of RE.
Management and Treatment Options

The management and treatment options for retrograde ejaculation depend on the underlying cause, the severity of the condition, and the individual’s fertility goals. Here are some common approaches to managing retrograde ejaculation:
- Medications: In cases where retrograde ejaculation is caused by medications, such as alpha-blockers used to treat high blood pressure, switching to an alternative medication may be recommended. Medications like pseudoephedrine or imipramine can sometimes be prescribed to help improve bladder neck muscle function and restore antegrade ejaculation. However, the effectiveness of these medications may vary among individuals.
- Fertility Treatments: For individuals or couples who are trying to conceive, assisted reproductive techniques can be used to overcome the fertility challenges posed by RE. These techniques include:
- Intrauterine Insemination (IUI): In IUI, sperm is collected from the urine after RE and processed in the laboratory. The prepared sperm is then inserted directly into the uterus during the woman’s fertile window, increasing the chances of fertilization.
- In Vitro Fertilization (IVF): IVF involves the collection of eggs from the woman and the retrieval of sperm from the urine or through testicular or epididymal sperm extraction (TESE). The eggs and sperm are fertilized in the laboratory, and the resulting embryos are transferred into the woman’s uterus.
- Nerve Stimulation Techniques: In some cases, electrical stimulation of the nerves responsible for ejaculation may be considered. This can be achieved through techniques such as penile vibratory stimulation or electroejaculation, which can help induce ejaculation and facilitate fertility treatments.
- Surgical Interventions: In certain cases, surgical interventions may be necessary, especially if RE is caused by structural abnormalities or previous surgeries. The specific surgical procedure will depend on the underlying cause and may involve repairing or reconstructing the bladder neck or related structures to restore normal ejaculation. However, surgical options are not always feasible or effective, and their use is determined on a case-by-case basis.
It is crucial to consult with a healthcare professional, such as a urologist or a reproductive endocrinologist, to determine the most appropriate treatment option based on individual circumstances. They will consider factors such as the underlying cause, the individual’s overall health, and fertility goals when developing a personalized treatment plan.
Patient Experience and Quality of Life
Many men with RE report that the condition has little impact on their overall quality of life or sexual satisfaction. However, the potential for infertility can understandably be a source of stress and concern, particularly for those wishing to conceive.
Moreover, the condition can sometimes contribute to feelings of embarrassment or self-consciousness. Therefore, it’s crucial to approach the topic with understanding and openness, and seek professional help if the condition is causing distress.
What Research Says: Recent Developments
Medical research has brought us a long way in understanding and managing RE. Recent studies have pointed towards the potential efficacy of certain medications in treating the condition. These drugs function by increasing the tone of the muscles at the bladder neck, thereby preventing the backward flow of semen.
Research has also focused on improving fertility treatments for men with RE, including advancements in sperm retrieval techniques and assisted reproductive technology.
As with any medical condition, staying informed about the latest research can empower you to make well-informed decisions about your health.
Living with Retrograde Ejaculation: Practical Tips
While retrograde ejaculation can seem daunting, here are some practical tips to manage the condition:
- Open Communication: Discuss your condition openly with your partner. This can help reduce stress and misunderstanding.
- Regular Check-ups: Regular visits to your healthcare provider can ensure optimal management of the condition, particularly if you’re looking to conceive.
- Stay Informed: Keeping up-to-date with the latest research can provide new insights into managing the condition and improving fertility outcomes.
Understanding retrograde ejaculation, its prognosis, and the various treatment options can go a long way towards managing the condition and maintaining a fulfilling sexual life. It’s essential to remember that while retrograde ejaculation might pose challenges, particularly regarding fertility, advances in medical science offer effective solutions.
Remember, every individual’s experience with retrograde ejaculation is unique. If you or someone you know is dealing with this condition, reach out to a healthcare professional who can provide personalized advice based on your specific circumstances.
While the journey may be daunting, remember that you’re not alone – and with knowledge, communication, and the right medical guidance, you can navigate the path to optimal sexual health and fertility.







































