What Is Peyronies Disease?

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

A Psychotherapist with Clinical specialization, working for over seven years now. Areas of specialization range from Anxiety-related disorders, Mood-related disorders, Personality disorders, Sexual dysfunctions & other mental health issues.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 11 November, 2023
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
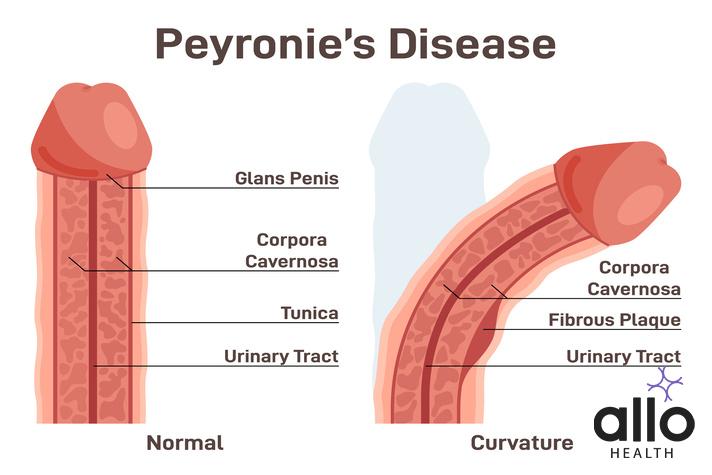
Peyronies disease is a condition that affects the penis and is named after Francois de la Peyronie, a French surgeon who first described the condition in 1743. Peyronie’s disease is also known as induratio penis plastica or IPP. It is a disorder in which the penis becomes curved (curved penis), often making it difficult to have sex or causing painful erections
Peyronie’s is a condition in which scar tissue, also known as plaque, forms inside the penis. This plaque can cause the penis to bend or curve when erect (abnormal curvature), and can also cause discomfort or pain during erection. The degree of curvature can vary from person to person, with some individuals experiencing only a slight bend, while others may experience a more severe curvature. Peyronie’s can also cause other symptoms, such as erectile dysfunction (ED) and a shortening of the penis.
Incidence & Prevalence Of Peyronie’s India
Peyronie’s is a relatively rare condition characterized by the development of fibrous scar tissue, or plaques, within the penis. These plaques can cause curvature, pain, and erectile dysfunction, leading to significant distress and discomfort for affected individuals. While there is limited specific data on the incidence and prevalence of Peyronie’s in India, we can provide some general information.
Incidence refers to the number of new cases of a particular condition diagnosed within a specific time period, usually expressed as a rate per population. Prevalence, on the other hand, refers to the total number of individuals living with a specific condition at a given time.
Due to the lack of comprehensive studies and registries specifically focused on Peyronie’s in India, precise incidence and prevalence rates for the country are not readily available. However, we can infer some estimates based on the limited global data and prevalence rates reported in other countries.
Globally, Peyronie’s is estimated to affect approximately 1-3% of adult males. It is more commonly observed in men aged 40 to 70, although it can occur at any age. It is important to note that these estimates are based on data from Western countries, and there may be regional variations.
In India, a study published in the Indian Journal of Urology in 2013 reported the prevalence of Peyronie’s to be around 0.6% among men seeking urological care in North India. This study was conducted at a single center and may not be representative of the entire country.
Furthermore, it is worth mentioning that Peyronie’s is often underreported and misdiagnosed due to its sensitive nature and the hesitance of individuals to seek medical attention for such conditions. This may contribute to an underestimation of the true incidence and prevalence.
To improve the understanding of Peyronie’s in India, further research and population-based studies are needed to provide more accurate estimates. These studies could involve larger sample sizes and include multiple centers across different regions of the country.
It is always recommended that individuals who suspect they may have Peyronie’s consult with a healthcare professional, such as a urologist, for a proper diagnosis and appropriate management.
Diagnosis Peyronie’s
 The diagnosis of Peyronie’s typically involves a combination of medical history assessment, physical examination, and sometimes additional tests.
The diagnosis of Peyronie’s typically involves a combination of medical history assessment, physical examination, and sometimes additional tests.
- Medical History: The healthcare provider will begin by taking a detailed medical history, including asking about the patient’s symptoms, the duration of symptoms, any previous injuries or surgeries to the penis, and any underlying medical conditions that may contribute to erectile dysfunction or penile abnormalities.
- Physical Examination: A physical examination is crucial for diagnosing Peyronie’s. The healthcare provider will visually inspect and palpate the penis to assess for any plaques or scar tissue. They may also evaluate the degree of penile curvature and the presence of pain or tenderness.
- Erection Assessment: To evaluate the extent of penile curvature, the healthcare provider may perform an assessment of the patient’s erection. This can be done by asking the patient to achieve an erection through sexual stimulation or by injecting a medication into the penis to induce an erection (intracavernosal injection). This helps determine the degree and direction of the curvature.
- Imaging Studies: In some cases, imaging studies may be ordered to provide a more detailed visualization of the penile plaques and curvature. These may include:
- Ultrasound: Ultrasound imaging, specifically penile Doppler ultrasound, can help identify the location and extent of the plaques and assess blood flow in the penis.
- Magnetic Resonance Imaging (MRI): MRI may be used in certain cases to evaluate the plaques and assess the degree of penile curvature. It provides detailed images of the soft tissues and can help determine the involvement of the underlying structures.
- Erectile Function Assessment: Peyronie’s can lead to erectile dysfunction (ED). If ED is present, the healthcare provider may conduct further assessments to evaluate its severity and underlying causes. This can involve additional tests, such as blood tests to check hormone levels, cavernosography, or nocturnal penile tumescence testing.
Symptoms Of Peyronie’s
Peyronie’s is characterized by the development of fibrous scar tissue, or plaques, within the penis. These plaques can cause a variety of symptoms, which may vary in severity from person to person.
- Penile Curvature: One of the hallmark symptoms of Peyronie’s is penile curvature. The scar tissue formation within the penis causes the affected area to become less flexible, leading to an abnormal curvature during erections. The curvature can be mild or severe, and it may be upward, downward, or to either side. The curvature can develop gradually or suddenly and may worsen over time.
- Pain or Discomfort: Many individuals with Peyronie’s experience pain or discomfort, particularly during erections or sexual activity. The pain may vary in intensity and can be described as a dull ache, sharp pain, or burning sensation. The pain is typically localized to the area where the plaques are present.
- Erectile Dysfunction (ED): Peyronie’s can also lead to erectile dysfunction, which is the inability to achieve or maintain an erection sufficient for sexual intercourse. The presence of the scar tissue can interfere with the normal blood flow within the penis, affecting the ability to achieve a rigid erection.
- Shortening of the Penis: In some cases, Peyronie’s can cause the penis to shorten. The formation of scar tissue can lead to the retraction of the affected area, resulting in a loss of penile length. This symptom may be more noticeable in individuals with severe or extensive plaque formation.
- Penile Indentation or Hourglass Deformity: In certain instances, the plaques in Peyronie’s can create an indentation or narrowing in the affected area of the penis. This can result in an hourglass-like deformity, where the penis appears constricted or pinched at the site of the plaque.
Risk Factors Of Peyronie’s
The exact cause of Peyronie’s is still not fully understood. However, several risk factors have been identified that may contribute to the development of the condition.
- Age: Peyronie’s most commonly affects men between the ages of 40 and 70. The risk of developing the condition tends to increase with age, although it can occur in younger men as well.
- Genetic Predisposition: There appears to be a genetic component to Peyronie’s, as it can sometimes run in families. Certain genetic factors may make some individuals more susceptible to developing the condition.
- Connective Tissue Disorders: Individuals with certain connective tissue disorders, such as Dupuytren’s contracture (a condition that causes the fingers to bend inward) or plantar fibromatosis (thickening of the tissue in the feet), have a higher risk of developing Peyronie’s. This suggests a possible association between these disorders and the development of fibrous plaques.
- Trauma or Injury: Previous trauma or injury to the penis has been identified as a potential risk factor for Peyronie’s. This includes activities or events that may cause penile fractures or repetitive injury, such as vigorous sexual intercourse or sports-related injuries.
- Penile Microtrauma: Microtrauma to the penis, which refers to small repetitive injuries over time, may contribute to the development of Peyronie’s. This can occur due to certain sexual practices or activities that involve aggressive bending or stretching of the penis.
- Penile Surgical Treatment or Procedures: Certain penile surgeries or procedures, such as prostate surgery, penile implants, or even repeated injections into the penis, have been associated with an increased risk of developing Peyronie’s.
- Smoking: Smoking tobacco is considered a risk factor for Peyronie’s. The toxins in cigarette smoke can damage blood vessels and impair tissue healing, potentially contributing to the development of scar tissue.
Treatment Of Peyronie’s
The treatment of Peyronie’s aims to alleviate symptoms, reduce penile curvature, and improve sexual function. The specific treatment options recommended by healthcare professionals may vary depending on the severity of symptoms, the progression of the , and individual patient factors.
- Observation: In mild cases of Peyronie’s where symptoms are minimal and do not significantly impact sexual function, healthcare providers may opt for a conservative approach of monitoring the condition without active treatment. Regular follow-up visits are typically scheduled to assess any changes in symptoms or disease progression.
- Medications: Several oral medications have been used in the treatment of Peyronie’s disease, although their effectiveness may vary among individuals. The two most commonly prescribed medications are:
- Collagenase Clostridium Histolyticum (CCH): CCH is an enzyme that breaks down the collagen present in the plaque, potentially reducing curvature. It is administered through a series of injections directly into the plaque. Multiple treatment cycles may be required.
- Potassium Para-Aminobenzoate (Potaba): Potaba is an oral medication that is thought to improve collagen metabolism. It is taken in the form of tablets multiple times a day for an extended period. The evidence for its effectiveness is mixed, and it may not be effective for all individuals.
- Intralesional Injections: Injections of certain medications directly into the plaque can be performed to soften the scar tissue, reduce pain, and potentially improve curvature. Verapamil, interferon-alpha-2b, and corticosteroids are examples of medications that may be used for this purpose.
- Extracorporeal Shockwave Therapy (ESWT): ESWT involves using high-frequency sound waves to break down the plaques and stimulate tissue healing. This non-invasive procedure is still being studied, and its long-term effectiveness is yet to be fully determined.
- Penile Traction Therapy: This therapy involves wearing a device that applies gentle and continuous stretching to the penis. It aims to reduce curvature and improve penile alignment over time. Penile traction therapy is usually used in combination with other treatments.
- Surgery: Surgical intervention may be considered in cases of severe curvature, significant penile deformity, or in individuals with erectile dysfunction that does not respond to other treatments. Surgical options include:
- Nesbit or Lue procedure: These procedures involve removing a portion of tissue opposite the plaque to correct the curvature.
- Penile prosthesis implantation: In cases where severe curvature and erectile dysfunction coexist, the placement of a penile prosthesis can address both concerns. It involves surgically implanting an inflatable or malleable device to enable erections.
- Psychological Support: Peyronie’s disease can have a significant psychological impact on individuals, leading to anxiety, depression, and reduced self-esteem. Psychological counseling or support may be beneficial in helping individuals cope with the emotional aspects of the condition.
Complications Of Peyronie’s
Peyronie’s disease can lead to several complications that can impact both physical and psychological well-being. Here are some of the potential complications associated with Peyronie’s disease:
- Erectile Dysfunction (ED): Peyronie’s disease can cause erectile dysfunction, which is the inability to achieve or maintain an erection sufficient for sexual intercourse. The presence of scar tissue and penile curvature can interfere with the normal blood flow within the penis, making it challenging to achieve a rigid erection.
- Pain and Discomfort: The fibrous plaques in Peyronie’s disease can cause pain and discomfort, particularly during erections or sexual activity. This can lead to a decreased desire for sexual intimacy and impact the overall quality of life.
- Penile Curvature: The most noticeable physical complication of Peyronie’s disease is penile curvature. The development of scar tissue can result in a bending or curvature of the penis during erections, which can make sexual intercourse difficult or even impossible.
- Penile Shortening: In some cases, Peyronie’s disease can cause penile shortening. The formation of scar tissue and the retraction of the affected area can lead to a loss of penile length. This can have a significant impact on body image and self-esteem.
- Psychological Distress: Peyronie’s disease can have a substantial psychological impact on affected individuals. The physical changes, including penile curvature and shortening, can lead to feelings of embarrassment, shame, and anxiety. These psychological factors can affect relationships, sexual confidence, and overall quality of life.
- Relationship concerns: The physical and psychological consequences of Peyronie’s disease can strain intimate relationships. The challenges associated with sexual function, pain during intercourse, and body image concerns can lead to communication difficulties, decreased sexual satisfaction, and relationship stress.
- Difficulty with Penetration and Intercourse: The curvature and deformity of the penis in Peyronie’s disease can make penetration during sexual intercourse challenging or even impossible. This can impact sexual satisfaction and may require adjustments in sexual positions or the exploration of alternative forms of intimacy.
Recurrence Of Curvature
Recurrence of curvature refers to the reappearance or worsening of penile curvature after treatment for Peyronie’s disease. While some treatment approaches aim to reduce or correct penile curvature, it’s important to note that Peyronie’s disease is a chronic condition, and recurrence of curvature can occur in some cases.
- Disease Progression: Peyronie’s disease is characterized by the formation of fibrous plaques in the penis. These plaques can progress or change over time, leading to recurrence or worsening of curvature. The underlying disease process may continue to cause the development of new plaques or enlargement of existing ones.
- Incomplete Correction: Treatment options such as surgery or collagenase injections aim to reduce or correct penile curvature. However, achieving complete correction may not always be possible. In some cases, there may be residual curvature after treatment, which can potentially lead to recurrence over time.
- Scar Tissue Elasticity: The scar tissue that develops in Peyronie’s disease is less elastic and flexible than normal penile tissue. Even with successful treatment, the scar tissue may retain some degree of rigidity. This rigidity can contribute to the recurrence of curvature, especially during erections when the penis becomes engorged with blood.
- Healing Response: The healing process in Peyronie’s disease can vary among individuals. Some individuals may have a more robust healing response, resulting in better resolution of curvature, while others may have a less favorable response, leading to recurrence or progression of curvature.
- Natural Disease Course: Peyronie’s disease is known for its variable and unpredictable nature. The condition can have periods of stability, where the curvature remains relatively unchanged, followed by periods of progression or recurrence. The exact reasons for these fluctuations in disease activity are not fully understood.
The recurrence of curvature does not necessarily indicate treatment failure. Each case of Peyronie’s disease is unique, and the recurrence of curvature can be influenced by various factors. If recurrence occurs, it is recommended to consult with a healthcare professional to reassess the condition, discuss treatment options, and address any ongoing concerns or symptoms.
Regular follow-up visits with a healthcare provider are crucial for monitoring the disease and managing any changes that may occur over time. By working closely with a healthcare professional, individuals with Peyronie’s disease can receive appropriate guidance and support in managing and minimizing the recurrence of curvature.
Urethral Injury And Peyronie’s Disease
Urethral injury and Peyronie’s disease are two separate conditions that can occur independently of each other. However, in some cases, urethral injury can be a potential risk factor or can occur concomitantly with Peyronie’s disease. Here’s a detailed explanation of the correlation between urethral injury and Peyronie’s disease:
- Urethral Injury: Urethral injury refers to damage or trauma to the urethra, the tube that carries urine from the bladder to the external opening of the penis. Urethral injuries can occur due to various causes, including trauma from accidents, pelvic fractures, catheter insertion, straddle injuries, or medical procedures involving the urethra.
- Peyronie’s Disease: Peyronie’s, as previously mentioned, is characterized by the development of fibrous scar tissue, or plaques, within the penis. These plaques can cause penile curvature, pain, and erectile dysfunction.
Correlation between Urethral Injury and Peyronie’s Disease
- Shared Risk Factors: Urethral injury and Peyronie’s disease may share some common risk factors. For example, trauma or injury to the penis or pelvic area can increase the risk of both urethral injury and the development of Peyronie’s. Additionally, certain medical procedures involving the urethra, such as urethral catheterization or urethral surgery, may pose a risk for both conditions.
- Concurrent Occurrence: In some cases, urethral injury and Peyronie’s disease can occur simultaneously. Trauma to the penis, particularly when it involves the urethra, can lead to the formation of scar tissue not only in the urethra but also in the penile tissues, resulting in Peyronie’s disease.
- Impact on Treatment and Outcomes: Urethral injury can complicate the management of Peyronie’s disease. Scar tissue from urethral injury can make surgical interventions for Peyronie’s disease more challenging, as it may affect the surgical approach and the overall success of the procedure.
It’s important to note that while there may be a correlation between urethral injury and Peyronie’s disease, it does not mean that one condition always leads to the other. Urethral injury and Peyronie’s disease can occur independently of each other and have their own unique causes and risk factors.
If you have experienced a urethral injury or suspect you have Peyronie’s disease, it is important to consult with a healthcare professional, such as a urologist, for an accurate diagnosis, appropriate treatment, and management options tailored to your specific condition.
Autoimmune Disorders And Peyronie’s Disease
The correlation between autoimmune disorders and Peyronie’s disease is not well understood. While Peyronie’s disease involves the formation of fibrous scar tissue within the penis, autoimmune disorders are characterized by an abnormal immune response that leads to the immune system attacking healthy tissues in the body. However, there are a few potential connections between autoimmune disorders and Peyronie’s disease that have been explored. Here’s a detailed explanation:
- Shared Immune Dysfunction: Both Peyronie’s disease and autoimmune disorders involve dysregulation of the immune system. In Peyronie’s disease, it is believed that an immune response triggered by injury or inflammation leads to the formation of fibrous plaques. Similarly, autoimmune disorders result from an overactive or misdirected immune response, causing immune cells to attack healthy tissues. It is possible that underlying immune dysfunction may contribute to the development or progression of Peyronie’s disease in some cases.
- Genetic Predisposition: Both autoimmune disorders and Peyronie’s disease are influenced by genetic factors. There is evidence to suggest a genetic component in the development of Peyronie’s disease, and certain autoimmune disorders also have a genetic predisposition. It is plausible that shared genetic factors or variations may contribute to an increased risk of developing both conditions in some individuals.
- Association with Specific Autoimmune Disorders: Some studies have reported an association between Peyronie’s disease and certain autoimmune disorders. For example, research has suggested a higher prevalence of Peyronie’s disease among individuals with Dupuytren’s contracture, which is characterized by the development of thickened fibrous tissue in the hands. Dupuytren’s contracture has been associated with autoimmune and inflammatory processes, indicating a potential link between autoimmune mechanisms and the development of Peyronie’s disease.
The exact relationship between autoimmune disorders and Peyronie’s disease is still not fully understood, and more research is needed to establish a definitive correlation. It is also worth mentioning that the majority of individuals with Peyronie’s disease do not have a diagnosed autoimmune disorder.
If you have an autoimmune disorder or suspect you have Peyronie’s disease, it is recommended to consult with a healthcare professional, such as a urologist or a specialist in autoimmune disorders, to assess your condition and provide appropriate management options tailored to your specific needs.
Mental Health And Peyronie’s Disease
The correlation between mental health and Peyronie’s disease is significant, as the condition can have a profound impact on a person’s emotional well-being and overall mental health. Here’s a detailed explanation of the correlation between mental health and Peyronie’s disease:
- Body Image and Self-Esteem: Peyronie’s disease can lead to physical changes in the penis, such as penile curvature, deformity, or shortening. These changes can significantly affect body image and self-esteem. Men may feel self-conscious, embarrassed, or ashamed about the appearance of their penis, which can have a negative impact on their mental well-being.
- Sexual Function and Intimacy: Peyronie’s disease can cause difficulties in sexual function, including pain during intercourse, erectile dysfunction, or challenges with penetration. These concerns can lead to frustration, anxiety, and decreased sexual satisfaction, which can affect an individual’s overall mental health and relationship dynamics.
- Psychological Distress: Dealing with the physical and functional changes associated with Peyronie’s disease can cause significant psychological distress. Individuals may experience feelings of sadness, frustration, anger, or anxiety. The distress can be further exacerbated by concerns about sexual performance, impact on relationships, and uncertainty about the future.
- Impact on Relationships: Peyronie’s disease can strain intimate relationships. The physical and emotional challenges associated with the condition may lead to difficulties in communication, reduced sexual intimacy, and relationship stress. These relationship dynamics can contribute to mental health concerns such as depression, anxiety, and decreased overall well-being.
- Coping with Emotional Impact: Managing the emotional impact of Peyronie’s disease is crucial for overall mental health. Individuals may benefit from seeking support from healthcare professionals, mental health counselors, or support groups. Addressing emotional concerns and developing effective coping strategies can help improve mental well-being and quality of life.
Frequently Asked Questions
Q1: What is Peyronie’s disease?
A1: Peyronie’s disease is a condition characterized by the development of fibrous scar tissue, known as plaque, within the penis. This plaque causes the penis to curve during erections, leading to pain, discomfort, and difficulties with sexual intercourse.
Q2: What are the symptoms of Peyronie’s disease?
A2: The primary symptom of Peyronie’s disease is the curvature of the penis. This curvature can vary in severity and may develop gradually or suddenly. Other symptoms include pain or tenderness during erections, the presence of lumps or hard tissue beneath the skin, and difficulties with achieving or maintaining an erection.
Q3: What causes Peyronie’s disease?
A3: The exact cause of Peyronie’s disease is not fully understood, but it is believed to result from trauma or injury to the penis. Microscopic tears in the penile tissue can trigger an inflammatory response, leading to the formation of scar tissue over time. Some risk factors for Peyronie’s disease include advancing age, genetic predisposition, and certain connective tissue disorders.
Q4: Can Peyronie’s disease be treated?
A4: Yes, there are several treatment options available for Peyronie’s disease. Mild cases may not require treatment and can improve on their own over time. However, if the curvature or other symptoms are bothersome, treatment options may include medication, such as collagenase injections or oral therapies, the use of penile traction devices, or surgery in severe cases.
Q5: Can Peyronie’s disease be cured?
A5: While Peyronie’s disease cannot be completely cured, treatment options can help manage the symptoms and reduce the curvature. Early intervention and treatment often yield better results. It is important to consult with a healthcare professional who can provide an accurate diagnosis and recommend the most appropriate treatment plan based on individual circumstances.
Q1: Is Peyronie’s disease a common condition?
A1: Peyronie’s disease is considered relatively common, affecting an estimated 3% to 9% of men. However, the actual prevalence may be higher, as many cases go unreported or undiagnosed due to embarrassment or the belief that it is a normal part of aging.
Q2: Can Peyronie’s disease go away on its own without treatment?
A2: In some cases, Peyronie’s disease may improve or stabilize without treatment. However, for many men, the condition does not resolve spontaneously. It is advisable to consult with a healthcare professional to determine the best course of action based on individual symptoms and circumstances.
Q3: Does Peyronie’s disease affect sexual function?
A3: Yes, Peyronie’s disease can impact sexual function. The curvature of the penis caused by the disease may make sexual intercourse difficult or painful. Some men may also experience erectile dysfunction or difficulties achieving and maintaining an erection due to the presence of scar tissue or psychological factors associated with the condition.
Q4: Can Peyronie’s disease lead to infertility?
A4: Peyronie’s disease itself does not typically cause infertility. However, the curvature and other symptoms associated with the condition can make sexual intercourse challenging, potentially affecting fertility if it hinders the delivery of semen into the vagina. If infertility concerns arise, it is important to consult with a fertility specialist who can assess and address any underlying concerns.
Q5: Can Peyronie’s disease be prevented?
A5: It is not possible to prevent Peyronie’s disease entirely, as its exact cause is still unknown. However, taking precautions to avoid penile injuries or trauma during sexual activity or other physical activities may help reduce the risk. It is also important to promptly address any penile pain or curvature changes to facilitate early diagnosis and treatment if Peyronie’s disease does develop.







































