Understanding the Pathology of Phimosis

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Dr. Aditi completed her undergraduate medical education at AJIMS, Mangalore, after which she worked in multi-speciality hospitals with COVID patients and in the Pain and Palliative medicine department. Driven by her experiences, she developed a keen interest in psychiatry. Dr. Aditi believes that mental health is just as, if not more important, than physical health.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 10 December, 2023
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
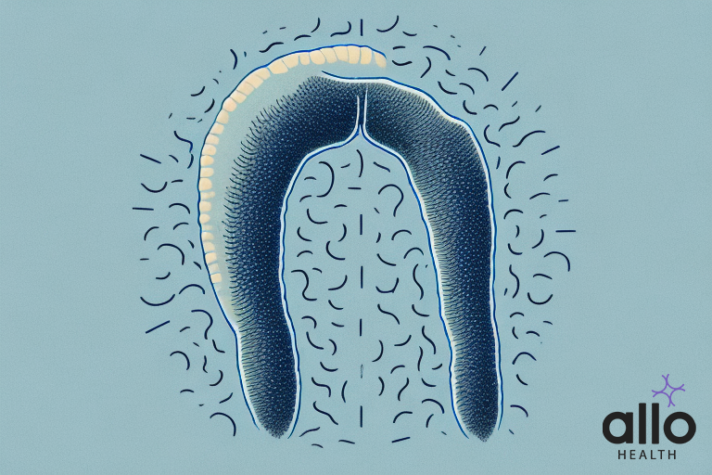
Phimosis is a medical condition that affects the foreskin of the penis, causing it to become tight and unable to retract. This condition is common in males, and can range in severity from mild to severe. Understanding the pathology behind phimosis is important in order to properly diagnose and treat it.
In this article, we will explore the various aspects of phimosis, including its types, causes, symptoms, diagnosis, and treatments.
What is Phimosis?
- Phimosis is a condition characterised by the tightness or narrowing of the foreskin of the penis, which makes it difficult or impossible to retract over the head of the penis.
- This can lead to discomfort, pain, and potential issues with hygiene.
- Phimosis can be a congenital condition (present from birth) or it can develop later in life due to factors like infection or inflammation.
Types of Phimosis
Phimosis can be classified into two main types:
Physiological Phimosis
Physiological phimosis is a common condition in infants and young boys where the foreskin is naturally tight and not fully retractable. It’s considered a normal developmental phase that often resolves on its own as the child grows.
Causes: Physiological phimosis occurs due to the gradual separation process between the foreskin and the glans penis. This separation takes time to complete, which is why it’s commonly observed in young boys.
Pathological Phimosis
Pathological phimosis is a condition where the foreskin is unable to retract due to an underlying issue inhibiting its natural separation from the glans. This condition can affect males of various age groups, including adolescents and adults. Several factors can lead to pathological phimosis:
- Scar Formation: Injuries, infections, or inflammation can result in the formation of scars, restricting the foreskin’s movement.
- Balanitis: This inflammatory condition of the glans and foreskin often arises from inadequate hygiene, infections, or specific medical conditions.
- BXO (Balanitis Xerotica Obliterans): A chronic and progressive condition characterised by white patches, scarring (stenosis scarring), and a narrowing of the foreskin opening.
- Infections: Recurrent or severe genital infections can lead to inflammation and a subsequent tightening of the foreskin.
- Trauma: Previous surgeries or injuries to the penis can induce scarring, potentially resulting in phimosis.

Signs and Symptoms of Phimosis
- Difficulty Retracting the Foreskin: One of the primary indicators of phimosis is the inability to retract the foreskin over the head of the penis.
- Tightness or Narrowing of the Foreskin Opening: The foreskin may appear constricted, making it challenging to expose the glans.
- Discomfort or Pain during Erection or Urination: Phimosis can lead to discomfort or pain, especially during activities like erections or urination.
- Redness and Swelling: Inflamed or irritated tissue around the foreskin may be noticeable, accompanied by redness and swelling.
- Recurrent Infections: Due to the difficulty in cleaning the area beneath the foreskin, individuals with phimosis may be more prone to infections.
- Balanitis or Balanoposthitis: Inflammation of the glans and foreskin, often caused by poor hygiene, infections, or certain medical conditions, can be a symptom of phimosis.
- Painful or Uncomfortable Sexual Activity: Phimosis can lead to discomfort or pain during sexual intercourse.
- White Patches or Scarring (in severe cases): In cases of advanced phimosis, white patches or scarring may be visible on the foreskin.
Children With Phimosis: Causes and Treatment
- In children, phimosis is relatively common, especially among infants and young boys. It occurs when the foreskin is naturally tight and not fully retractable, which is considered a normal developmental phase.
- In most cases, this condition resolves on its own as the child grows, without the need for medical intervention.
- If phimosis persists or causes discomfort, mild cases can often be effectively treated with non-invasive methods like steroid creams.
- Severe cases may require more advanced treatments, and in rare instances, surgical intervention may be considered.
- It’s important to consult a healthcare professional for tailored advice and appropriate management.
What Increases Risk of Phimosis?
- Uncircumcised Males: Individuals who have not undergone circumcision are at a higher risk of developing phimosis. This is because the foreskin remains intact and may be more prone to conditions that lead to phimosis.
- History of Balanitis or Balanoposthitis: Previous episodes of balanitis (inflammation of the glans) or balanoposthitis (inflammation of the glans and foreskin) can lead to scarring and increase the likelihood of developing phimosis.
- Infections: Recurrent or chronic infections in the genital area can contribute to the development of phimosis. These infections may lead to scarring and tightening of the foreskin.
- Trauma or Injury: Previous trauma or injury to the penis, such as accidents or surgical procedures, can result in scarring that leads to phimosis.
- Inadequate Hygiene Practices: Poor hygiene habits can lead to the accumulation of smegma (a natural substance) beneath the foreskin. This can cause irritation and inflammation, potentially contributing to phimosis.
- Autoimmune Conditions: Certain autoimmune conditions or inflammatory disorders may increase the risk of developing phimosis. Conditions like lichen sclerosus (BXO) are known to be associated with phimosis.
- Genetic Predisposition: There may be a genetic component to phimosis, meaning that individuals with a family history of the condition may be at a higher risk.
- Age and Hormonal Changes: Older individuals may experience changes in the elasticity of the foreskin, potentially leading to phimosis.
While these factors can increase the risk of developing phimosis, it does not guarantee its occurrence.
Diagnosis of Phimosis
Assessment of Phimosis (Clinical Evaluation):
- Physical Examination: A healthcare provider will conduct a thorough examination of the genital area. They will assess the appearance of the foreskin, its ability to retract, and any signs of inflammation or scarring.
- Medical History: Gathering information about any previous episodes of balanitis, infections, or injuries to the genital area is crucial in understanding the context of the condition.
Additional Tests or Procedures:
- Swabs or Cultures (if infection is suspected): In cases where recurrent infections are a concern, swabs or cultures may be taken to identify specific pathogens and guide treatment.
- Biopsy (if BXO is suspected): If Balanitis Xerotica Obliterans (BXO) is suspected, a small tissue sample may be taken for examination under a microscope to confirm the diagnosis.
- Specialised Imaging (rare): In rare cases where there are complications or underlying concerns, specialised imaging tests such as ultrasound or magnetic resonance imaging (MRI) may be recommended.
Referral to a Specialist:
In some cases, particularly when the diagnosis is unclear or the condition is severe, a referral to a urologist or a dermatologist with expertise in genital conditions may be advised.
Treatment of Phimosis
Topical Steroid Creams:
- Mild cases of phimosis can often be treated with prescription-strength steroid creams. These creams work by reducing inflammation and promoting the elasticity of the foreskin.
- The cream is applied directly to the narrowed part of the foreskin, and a healthcare provider will provide specific instructions on its use.
Manual Stretching:
- This involves gently stretching the foreskin over a period of time. It can be done by the individual or with the guidance of a healthcare professional.
- It’s crucial to do this with care and not force the foreskin, as excessive force can lead to injury.
Preputioplasty:
- This is a minor surgical procedure that involves making a small incision in the foreskin to widen the opening. It’s an effective option for cases where conservative treatments are not successful.
- Preputioplasty preserves the foreskin, which may be important to some individuals.
Circumcision:
- Some patients with phimosis opt for the surgical removal of the foreskin. It’s a more definitive solution for severe or recurrent cases of phimosis.
- Circumcision is a permanent procedure, so it’s important for individuals to carefully weigh the benefits and potential drawbacks.
Post-Surgical Care:
- After any surgical intervention, it’s crucial to follow post-operative care instructions provided by the healthcare provider to ensure proper healing and minimise the risk of complications.
Follow-Up and Monitoring:
- Regular follow-up appointments with a healthcare provider are important to monitor progress and address any concerns or complications that may arise during the treatment process.
Prognosis of Phimosis
- The prognosis of phimosis largely depends on its severity and the chosen treatment approach.
- In cases of physiological phimosis, which is common in infants and young boys, the condition often resolves naturally as the child grows.
- Mild cases may respond well to non-invasive treatments like topical steroid creams or manual stretching, with a favourable prognosis.
- If left untreated or if conservative methods are unsuccessful, more severe cases may lead to complications such as recurrent infections or discomfort during sexual activity. In such instances, surgical options like preputioplasty or circumcision may be recommended, providing a long-term solution with a positive prognosis for improved genital health and comfort.
- It’s important for individuals to seek timely medical advice and explore the most appropriate treatment option under the guidance of a healthcare professional.
Prevention of Phimosis
- Maintain Good Hygiene: Regularly clean the genital area, including under the foreskin, to prevent the buildup of smegma (natural oils and dead skin cells).
- Teach Proper Cleaning Techniques: Educate young boys and adolescents on how to clean the genital area during bath or shower routines.
- Avoid Harsh Soaps and Chemicals: Use mild, fragrance-free soaps and avoid harsh chemicals or products that may irritate the sensitive genital skin.
- Treat Infections Promptly: Seek prompt medical attention for any infections in the genital area to prevent potential scarring and complications.
- Practice Safe Sex: Engage in safe sexual practices to reduce the risk of sexually transmitted infections, which can lead to inflammation and scarring.
- Avoid Trauma or Injury: Take precautions to prevent accidents or injuries to the genital area, and seek immediate medical attention if any occur.
- Consider Circumcision: Some individuals may choose circumcision as a preventive measure, although this is a personal decision and should be discussed with a healthcare provider.
- Regular Check-Ups: Schedule routine medical check-ups to monitor genital health and address any concerns promptly.
- Seek Medical Advice for Persistent Symptoms: If there are any signs of discomfort, tightness, or difficulty retracting the foreskin, consult a healthcare professional for proper evaluation and guidance.
Key Takeaways
- Phimosis is a condition where the foreskin of the penis is tight, causing difficulty in retraction.
- Types of phimosis include physiological (common in young boys) and pathological (due to underlying issues).
- Signs of phimosis include difficulty retracting foreskin, discomfort, redness, and potential infections.
- Risk factors include uncircumcised status, history of infections, and autoimmune conditions.
- Prevention involves hygiene, safe practices, and seeking prompt medical advice for symptoms.
Frequently Asked Questions
Q: What is paraphimosis?
A: Paraphimosis is a medical condition where the retracted foreskin of the penis cannot be returned to its original position, causing constriction and potential complications. It requires prompt medical attention to prevent further concerns.
Q: What is congenital phimosis?
A: Congenital phimosis is a condition present from birth where the foreskin of the penis is naturally tight and not fully retractable. It’s considered a normal developmental phase in infants and young boys.
Q: What are the symptoms of Balanitis include?
A: Symptoms of Balanitis include redness, swelling, and irritation of the head of the penis (glans). It may also involve discomfort, itching, and a discharge in some cases.
Q: Is phimosis treatment for children the same as adult males?
A: Treatment procedure in children and adults for phimosis may vary. While mild cases in children often resolve naturally, adults may require treatments like steroid creams or surgical options depending on the severity. Consulting a healthcare professional is essential for tailored advice.
Q: Is erection with phimosis possible?
A: Yes, it is possible to experience an erection with phimosis. However, in some cases, especially if it’s severe phimosis, it may cause discomfort or pain during erections. Consulting a healthcare professional for proper evaluation and guidance is advised.






































