What Is ICD-10 Code For Phimosis?

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Dr Sanina Mansoor holds MBBS degree from Yenepoya university,Mangalore.She has 8 years of experience working as a medical officer at various health centres and medical colleges.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 20 December, 2023
- Article was updated as part of our commitment to diversity, equity, and inclusion.

"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
Phimosis is a medical condition that affects men, and can cause significant pain and discomfort. It occurs when the foreskin of the penis is too tight to retract over the glans, or head, of the penis. This can cause concerns with hygiene, urination, and sexual intercourse.
What Is Phimosis?
Phimosis is a medical condition that primarily affects males, involving the foreskin of the penis. The foreskin is a fold of skin that covers the head (glans) of the penis in males who have not undergone circumcision. Phimosis occurs when the opening of the foreskin is too tight to be retracted over the glans, making it difficult or impossible to expose the head of the penis.
There are two main types of phimosis:
- Physiological Phimosis: This is considered normal in infants and young children. Newborn boys usually have a tight foreskin that gradually becomes more flexible and retractable as they grow. By the age of 3 to 5, most boys can retract their foreskin comfortably. This type of phimosis typically resolves naturally with time and proper hygiene practices.
- Pathological Phimosis: This type of phimosis is a medical condition that occurs in older boys and adult men. It may result from various causes, including:
- Scarring or inflammation: Infections, poor hygiene, or irritation can lead to scarring and inflammation of the foreskin, causing it to tighten and become less flexible.
- Balanitis: Inflammation of the glans and foreskin, often caused by infection or poor hygiene, can contribute to phimosis.
- Trauma: Injuries to the genital area can lead to scarring and tightening of the foreskin.
- Medical conditions: Certain medical conditions like lichen sclerosis or diabetes can increase the risk of developing phimosis.
Types of Phimosis: Congenital vs Acquired
Phimosis is categorized into two main types based on its origin and onset: congenital phimosis and acquired phimosis. Let’s explore each type in detail:
Congenital Phimosis
Congenital phimosis is present from birth and is considered a normal developmental stage in infants and young children. In this type of phimosis, the foreskin is naturally tight and does not fully retract over the glans (head) of the penis. This condition is typically harmless and often resolves on its own as the child grows older.
Causes:
- During fetal development, the foreskin is attached to the glans. Over time, natural separation occurs, allowing the foreskin to gradually become more retractable. This process can take several years to complete.
Characteristics:
- Congenital phimosis is commonly observed in newborn boys.
- It is a normal and transient condition in infancy.
- Most cases of congenital phimosis resolve naturally without the need for medical intervention.
- The tightness of the foreskin decreases as the child grows older, and the opening becomes more flexible.
Acquired Phimosis
Acquired phimosis develops after the newborn period and is usually the result of various factors such as infection, inflammation, or trauma. Unlike congenital phimosis, acquired phimosis is often associated with discomfort and may require medical attention.
Causes:
- Infections: Bacterial or fungal infections in the genital area can cause inflammation and scarring of the foreskin, leading to acquired phimosis.
- Poor hygiene: Inadequate cleaning of the penis can lead to the buildup of smegma (a mixture of dead skin cells and bodily fluids) under the foreskin, causing irritation and inflammation.
- Balanitis: Inflammation of the glans and foreskin can contribute to acquired phimosis.
- Trauma: Injuries to the genital area can cause scarring and tightening of the foreskin.
- Medical conditions: Conditions like lichen sclerosis, a chronic inflammatory skin disorder, can result in acquired phimosis.
Characteristics:
- Acquired phimosis usually develops in older children, adolescents, and adult men.
- It often causes discomfort, pain, and difficulty retracting the foreskin.
- If left untreated, acquired phimosis can lead to complications such as urinary tract infections, balanitis, and sexual dysfunction.
Symptoms of Phimosis
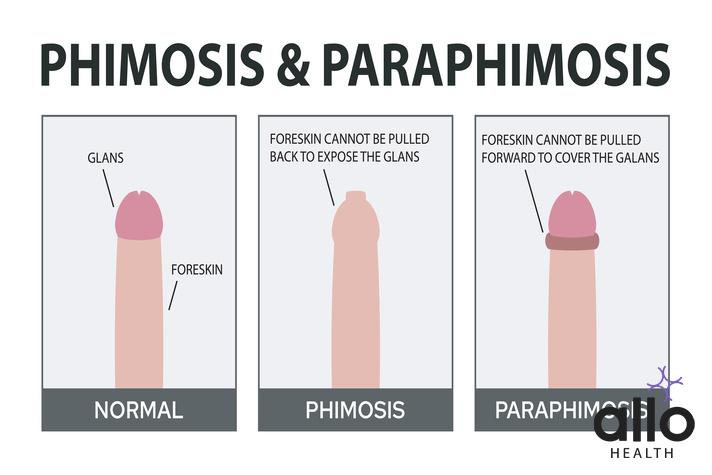
Phimosis is a condition where the foreskin of the penis is too tight to be retracted over the glans (head) of the penis. The symptoms of phimosis can vary depending on the severity of the condition and whether it is congenital or acquired. Here are the symptoms in detail:
Congenital Phimosis
In infants and young children with congenital phimosis, the symptoms may include:
- Non-retractable Foreskin: The most common symptom of congenital phimosis is the inability to retract the foreskin over the glans of the penis. This is considered normal in infants and young children and usually resolves on its own over time.
- Redness and Irritation: The tightness of the foreskin can lead to redness, irritation, and discomfort around the head of the penis.
- Difficulty Urinating: In some cases, the tight foreskin might cause difficulty in urination, such as a ballooning of the foreskin during urination.
- Pain or Discomfort: If the foreskin becomes particularly tight, it might cause pain or discomfort for the child.
Acquired Phimosis
In older children, adolescents, and adult men with acquired phimosis, the symptoms may include:
- Difficulty Retracting the Foreskin: The most common and prominent symptom of acquired phimosis is the difficulty or inability to retract the foreskin. This might be partial or complete. Attempting to forcefully retract the foreskin can lead to pain and further complications.
- Pain and Discomfort: Trying to retract the tight foreskin can cause pain, discomfort, and even tearing of the skin.
- Inflammation and Swelling: The area under the foreskin might become inflamed, red, and swollen due to irritation or infection.
- Balanitis: Balanitis is the inflammation of the glans and foreskin. It can be caused by poor hygiene, infections, or irritation resulting from the presence of smegma (a mixture of dead skin cells and bodily fluids) under the foreskin.
- Urinary concerns: Acquired phimosis can lead to difficulties in urination, such as a weakened urine stream or difficulty fully emptying the bladder.
- Hygiene Concerns: The inability to retract the foreskin can lead to hygiene concerns, as cleaning the area beneath the foreskin becomes challenging. This can result in the accumulation of debris, leading to further inflammation and infection.
- Painful Erections or Sexual Intercourse: In severe cases, acquired phimosis might cause pain during erections or sexual intercourse.
While congenital phimosis in infants and young children is usually considered a normal developmental stage that often resolves on its own, acquired phimosis in older individuals might require medical attention. If you or someone you know is experiencing symptoms of phimosis, it’s recommended to consult a healthcare provider for proper diagnosis and appropriate treatment options.
Causes of Phimosis
Phimosis is a condition where the foreskin of the penis is too tight to be retracted over the glans (head) of the penis. There are different causes of phimosis, and they can be classified into two main categories: congenital (present from birth) and acquired (developed after birth). Here are the causes of phimosis in detail:
Congenital Causes
- Normal Development: In many newborn boys, the foreskin is naturally tight and adhered to the glans. This is a normal developmental stage and is considered congenital phimosis. Over time, as the child grows, the foreskin typically becomes more retractable, and this type of phimosis often resolves on its own without intervention.
Acquired Causes
- Poor Hygiene: One of the most common acquired causes of phimosis is poor hygiene. Inadequate cleaning of the penis can lead to the buildup of smegma, a mixture of dead skin cells and bodily fluids, under the foreskin. This buildup can cause irritation, inflammation, and scarring, leading to a tight foreskin.
- Infections: Infections of the genital area, such as bacterial or fungal infections, can cause inflammation and scarring of the foreskin. These infections can be the result of poor hygiene or other factors and contribute to acquired phimosis.
- Balanitis: Balanitis is the inflammation of the glans and foreskin. It can be caused by poor hygiene, irritation, or infections. Balanitis can lead to swelling and scarring of the foreskin, resulting in phimosis.
- Trauma: Injuries to the genital area, such as from accidents, rough handling, or aggressive cleaning, can cause scarring and tightening of the foreskin, leading to acquired phimosis.
- Medical Conditions: Certain medical conditions can increase the risk of developing acquired phimosis. For example, lichen sclerosis is a chronic inflammatory skin disorder that can cause white, patchy areas of skin on the genitals and lead to tightening of the foreskin.
- Recurrent Balanoposthitis: Balanoposthitis is inflammation of both the glans and foreskin. If someone experiences repeated episodes of this condition, it can lead to scarring and phimosis.
- Inflammatory Skin Disorders: Other inflammatory skin conditions, such as psoriasis or eczema, can affect the genital area and contribute to acquired phimosis.
The severity of phimosis can vary based on the underlying cause. Mild cases of acquired phimosis might be managed with conservative measures and proper hygiene, while more severe cases might require medical intervention such as topical steroid creams or surgical procedures like circumcision or preputioplasty.
Diagnosis of Phimosis: ICD-10 Code
In the International Classification of Diseases, 10th Revision (ICD-10), phimosis is classified under the category “N47 Other disorders of the foreskin” within Chapter XIV “Diseases of the genitourinary system (N00-N99).” The ICD-10 code for phimosis is N47.1. Let’s break down the diagnosis and its corresponding code in more detail:
ICD-10 Code: N47.1
Description: Other disorders of the foreskin (N47) includes a variety of conditions affecting the foreskin of the penis, including phimosis. The specific code for phimosis is N47.1. This code is used to indicate the presence of phimosis and is essential for medical documentation, billing, and coding purposes.
Diagnostic Criteria for Phimosis:
- Clinical Examination: The diagnosis of phimosis is typically made through a clinical examination by a healthcare provider. The following criteria are often used to diagnose phimosis:
- The inability to retract the foreskin fully over the glans (head) of the penis.
- Tightness or narrowing of the foreskin opening.
- Presence of symptoms such as discomfort, pain, inflammation, or difficulty urinating.
- Medical History: The healthcare provider may inquire about the patient’s medical history, including any previous episodes of balanitis (inflammation of the glans and foreskin), infections, or trauma that might contribute to the development of phimosis.
- Underlying Causes: If the phimosis is acquired and not congenital, the healthcare provider might investigate potential underlying causes such as poor hygiene, infections, or inflammatory skin conditions.
Use of ICD-10 Code N47.1:
When a healthcare provider diagnoses a patient with phimosis, they would use the ICD-10 code N47.1 to classify and document the condition. This code is used for medical records, insurance claims, research purposes, and communication between healthcare professionals.
Accurate diagnosis and proper treatment recommendations should be provided by a qualified healthcare provider. If you suspect you or someone you know has phimosis, seeking medical attention is crucial for a proper assessment, diagnosis, and appropriate management of the condition.
Treatment Options for Phimosis
The treatment for phimosis depends on factors such as the underlying cause, the severity of the condition, the patient’s age, and their overall health. There are both conservative and medical/surgical treatment options available. Here are the treatment options for phimosis in detail:
Conservative Management
For cases of phimosis that are not causing significant discomfort or complications, and especially in cases of physiological phimosis in infants and young children, conservative approaches may be tried:
- Regular Hygiene: Proper hygiene is essential to prevent inflammation and infection. Gently cleaning the penis and the area under the foreskin during bathing can help prevent buildup of smegma and maintain good genital health.
- Topical Steroid Creams: In acquired phimosis cases with inflammation, a doctor may prescribe a topical steroid cream, such as hydrocortisone. The cream can help reduce inflammation and soften the foreskin, making it easier to retract over time. This option is most effective for mild to moderate cases of acquired phimosis.
- Gradual Stretching: Under medical supervision, gentle stretching of the foreskin over time can help increase its flexibility. This is often done using the fingers and is more effective when combined with the use of a topical steroid cream.
Medical Interventions
If conservative approaches are not effective or the condition is causing discomfort and complications, medical interventions may be recommended:
- Surgical Treatments: Surgical options are considered when conservative measures fail. The two main surgical procedures are circumcision and preputioplasty.
- Circumcision: This involves the surgical removal of the foreskin. It is a definitive solution to phimosis, and it eliminates the risk of recurrence. Circumcision is a more invasive option and is typically reserved for cases where other treatments have not been successful or when other medical conditions warrant it.
- Preputioplasty: This is a less invasive surgical procedure that involves making small incisions in the tight part of the foreskin to enlarge the opening. Unlike circumcision, preputioplasty preserves most of the foreskin while alleviating the phimosis.
- Dorsal Slit: In some cases, a dorsal slit procedure may be performed. This involves making a vertical incision along the tight portion of the foreskin to relieve the constriction.
- Partial Frenuloplasty: If the tightness is primarily due to a short frenulum (the band of tissue connecting the foreskin to the glans), a partial frenuloplasty might be considered. This procedure involves releasing the frenulum to improve foreskin retraction.
Consult a healthcare provider to determine the most appropriate treatment option based on the individual’s specific condition. Self-diagnosis and self-treatment should be avoided, as they can lead to complications. A healthcare provider can provide a proper diagnosis, discuss the potential benefits and risks of each treatment option, and help make an informed decision regarding the best course of action for managing phimosis.
Frequently Asked Questions
(1) What is the ICD-10 code for phimosis?
The ICD-10 code for phimosis is N47.1. This code is used to classify and document cases of phimosis, a condition where the foreskin is too tight to retract over the head of the penis.
(2) How is phimosis diagnosed using the ICD-10 code?
Healthcare providers use the ICD-10 code N47.1 when diagnosing and documenting cases of phimosis. This code helps in medical records, billing, and communication among healthcare professionals.
(3) Is phimosis a common condition?
Yes, phimosis is relatively common, especially in infants and young boys. In many cases, it’s a normal developmental stage that resolves as the child grows older.
(4) Can phimosis be treated without surgery?
Yes, milder cases of phimosis can often be managed without surgery. Conservative treatments like proper hygiene, topical steroid creams, and gentle stretching exercises under medical guidance are commonly used.
(5) When might surgery be considered for phimosis?
Surgery, such as circumcision or preputioplasty, is considered when conservative measures are not effective, or when phimosis causes discomfort, pain, or complications that impact daily life.
(6) Is phimosis only an concern for infants and children?
No, phimosis can affect individuals of all ages. While congenital phimosis is common in infants, acquired phimosis can develop in adolescents and adults due to factors like infections, poor hygiene, and inflammation.
(7) Can phimosis lead to serious complications?
Untreated or severe cases of phimosis can lead to complications such as infections, balanitis, urinary concerns, and pain during sexual activity. Seeking medical attention is important if complications arise.
(8) Can phimosis cause difficulties in urination?
Yes, in some cases, the tight foreskin can lead to difficulties in urination, including a weakened urine stream or difficulties fully emptying the bladder.
(9) Is circumcision the only surgical option for phimosis?
No, besides circumcision, there are other surgical options like preputioplasty and dorsal slit procedures. These options are considered based on individual circumstances and severity of phimosis.
(10) How can I know if I have phimosis?
If you have difficulty retracting the foreskin, experience discomfort, pain, inflammation, or other genital concerns, it’s recommended to consult a healthcare provider. They can diagnose phimosis and recommend appropriate treatments based on your specific condition.






































