History of endometriosis ICD 10
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
Endometriosis is a complex and often misunderstood condition that affects millions of women worldwide. Its history dates back to ancient times, with the first recorded cases described in medical texts from Egypt and Greece. However, it wasn’t until the 19th century that endometriosis began to be studied in earnest. In this article, we’ll explore the history of endometriosis diagnosis and treatment, with a particular focus on the current International Classification of Diseases (ICD) coding system: ICD 10.
Understanding Endometriosis: Definition, Symptoms, and Causes
Endometriosis is a chronic condition where the tissue that normally lines the uterine body grows outside of it, causing inflammation, pain, and often infertility. Its symptoms can include heavy and painful periods, chronic pelvic pain, pain during sex, and difficulties with fertility. The causes of endometriosis are still not fully understood, but it is believed to be linked to genetics, hormonal imbalances, and environmental factors.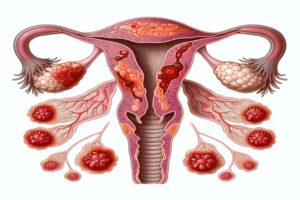
Recent studies have also suggested a possible link between endometriosis and autoimmune disorders. Women with the incidence of endometriosis have been found to have a higher risk of developing autoimmune diseases such as lupus, multiple sclerosis, myeloproliferative disorders and rheumatoid arthritis. This has led researchers to investigate the role of the immune system in the development and progression of endometriosis.
The Diagnostic Criteria for Endometriosis: From ICD 9 to ICD 10
Endometriosis has undergone significant changes in its diagnostic criteria over the past few decades. In 1975, the American Fertility Society (AFS) developed an endometriosis classification system based on the extent and severity of the disease. This classification was later revised in 1985 and 1997. Then in 2015, the World Health Organization (WHO) released ICD-10-CM Diagnosis Code, which replaced the previous diagnostic codes, ICD 9.
The new ICD 10 criteria for endometriosis diagnosis includes a more detailed classification system that takes into account the location, depth, and size of the endometrial tissue growths. This allows for a more accurate diagnosis and better understanding of the disease. Additionally, the new criteria also includes specific codes for associated symptoms such as chronic pelvic pain and infertility.
Despite the improvements in diagnostic criteria, endometriosis remains a challenging disease to diagnose and treat. Many women with endometriosis experience long delays in diagnosis and inadequate treatment. It is important for healthcare providers to be aware of the updated diagnostic criteria and to listen to their patients’ symptoms and concerns in order to provide the best possible care.
The Evolution of Endometriosis Diagnosis: A Timeline of ICD Codes
The history of endometriosis diagnosis is a fascinating one. From the earliest recorded cases in ancient Egypt and Greece to the development of the AFS classification system, it has undergone significant changes over time. The most recent change came in 2015, when the WHO released ICD-10-CM codes for endometriosis. This new coding system has been a significant step forward in the diagnosis and classification of endometriosis and other disorders of the genital tract and pelvic peritoneum.
ICD 10 has allowed for more accurate and specific diagnosis of endometriosis. It includes codes for deep infiltrating endometriosis, ovarian endometriomas, and adenomyosis, which were not previously included in the classification system. This has led to improved understanding and treatment of the disease, as well as better tracking of its prevalence and impact on individuals and society as a whole.
Endometriosis Across the Globe: An Epidemiological Overview
Endometriosis is a global problem, affecting an estimated 10% of women of reproductive age worldwide. However, its prevalence varies widely between regions and countries. In this section, we’ll explore the epidemiology of endometriosis and its impact on women’s health across the globe along with its malignant potential.
Recent studies have shown that endometriosis is more prevalent in developed countries, such as the United States and Europe, compared to developing countries. This may be due to differences in healthcare access and awareness, as well as lifestyle factors. Additionally, women with a family history of endometriosis are at a higher risk of developing the condition themselves and so should be pertinent in their follow-up examination. It is important for healthcare providers to recognize the global impact of endometriosis and work towards improving diagnosis and treatment options for all women affected by this condition.
Risk Factors for Endometriosis: Genetics, Lifestyle, and Environmental Factors
Endometriosis is a complex condition that can be influenced by a range of genetic, lifestyle, and environmental factors. In this section, we’ll take a closer look at the risk factors associated with endometriosis and what they tell us about the condition’s underlying causes and risk of endometriosis.
One of the most significant risk factors for endometriosis is a family history of the condition. Studies have shown that women with a first-degree relative (such as a mother or sister) who has endometriosis are up to seven times more likely to develop the condition themselves. This suggests that there may be a genetic component to endometriosis along with other socioeconomic factors and reproductive factors, although the specific genes involved have not yet been identified.
The Link between Endometriosis and Infertility: What You Need to Know
Infertility is a common complication of endometriosis, affecting up to 50% of women with the condition. It is caused by the way that abnormal endometrial tissue growth can interfere with the reproductive organs. In this section, we’ll explore the link between endometriosis and infertility and the treatment options available for women who are trying to conceive.
It is important to note that not all women with endometriosis will experience infertility. Factors such as the severity and location of the endometrial tissue growth, as well as the age of the woman and associated adult characteristics, can all play a role in determining the likelihood of infertility. Additionally, there are various fertility treatments available for women with endometriosis, including in vitro fertilization (IVF) and surgery to remove the endometrial tissue. It is important for women with endometriosis who are trying to conceive to work closely with their healthcare provider to determine the best course of action.
Endometriosis Staging Systems: A Comparison of ASRM and ENZIAN Classification
Endometriosis is a complex and difficult-to-stage disease. Over the years, several classification systems have been developed to help doctors assess the extent and severity of the disease. In this section, we’ll take a closer look at two of the most commonly used endometriosis staging systems: the American Society of Reproductive Medicine (ASRM) and the the Enzian classification system.
The ASRM classification system is based on the location, extent, and depth of endometrial implants, as well as the presence and severity of adhesions and ovarian cysts. It uses a point system to assign a stage to the disease, ranging from stage I (minimal disease) to stage IV (severe disease). This system is widely used in clinical practice and research, and it allows for standardized communication among healthcare providers.
The Enzian classification system, on the other hand, focuses on the morphology and histology of endometrial implants, as well as the presence of fibrosis and inflammation. It uses a letter system to assign a stage to the disease, ranging from stage A (superficial disease) to stage D (deep infiltrating disease). This system is less commonly used than the ASRM system, but it may be more useful in cases where the extent of the disease is not well-defined or when the disease is located in unusual sites.
The Role of Imaging Techniques in Diagnosing Endometriosis: Ultrasound, MRI, and CT Scan
Imaging techniques are often used in the diagnosis of endometriosis, particularly in cases where laparoscopy is not an option. In this section, we’ll explore the role of ultrasound, MRI, and CT scans in diagnosing endometriosis and the advantages and limitations of each technique and their role in the care of endometriosis patients.
Ultrasound is a commonly used imaging technique in the diagnosis of endometriosis. It is non-invasive and relatively inexpensive, making it a preferred option for many patients. However, ultrasound may not be able to detect all cases of endometriosis, particularly in cases where the lesions are small or located in hard-to-reach areas. MRI and CT scans, on the other hand, are more sensitive and can detect endometriosis in areas that may be missed by ultrasound. However, these techniques are more expensive and may not be readily available in all healthcare settings. Ultimately, the choice of imaging technique will depend on the individual patient’s needs and the expertise of the healthcare provider.
Laparoscopy for Endometriosis Treatment: An Overview of the Procedure and Outcomes
Laparoscopy is a minimally invasive surgical procedure that is commonly used to diagnose and treat basis of endometriosis and other reproductive system disorders. In this section, we’ll take a closer look at what the procedure involves and what you can expect in terms of outcomes and recovery.
During a laparoscopy for endometriosis treatment, a small incision is made in the abdomen and a thin, lighted tube with a camera attached (laparoscope) is inserted. The surgeon can then view the pelvic organs and identify any endometrial tissue growths. If endometriosis is found, the surgeon can remove the tissue using specialized surgical instruments. Recovery time after the procedure is typically shorter than with traditional open surgery, with most patients able to return to normal activities within a week or two with successful ambulatory encounters.
Medical Management of Endometriosis Pain: Hormonal Therapy and Pain Relievers
Medical management is often the first line of treatment for endometriosis pain. In this section, we’ll explore the range of hormone therapies and pain relievers available to women with endometriosis and their effectiveness in managing symptoms.
Hormonal therapy is a common treatment option for endometriosis pain. It works by suppressing the production of estrogen, which can reduce the growth and spread of endometrial tissue. Hormonal therapy can be administered in the form of birth control pills, patches, injections, or intrauterine devices (IUDs). Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can also be used to manage endometriosis pain. These medications work by reducing inflammation and blocking the production of prostaglandins, which are chemicals that cause pain and inflammation. However, it’s important to note that pain relievers only provide temporary relief and do not address the underlying cause of endometriosis.
Surgical Treatment Options for Endometriosis: Excision, Ablation, and Hysterectomy
Surgery is often required to treat severe cases of endometriosis. There are several surgical options available, including excision, ablation, and hysterectomy. In this section, we’ll explore these surgical techniques, their indications, and their outcomes.
It is important to note that surgery is not always the first line of treatment for endometriosis. In less severe cases, hormonal therapy or pain management may be recommended before considering surgery. However, for women with severe symptoms or those who have not responded to other treatments, surgery may be necessary.
Alternative Therapies for Endometriosis Management: Acupuncture, Yoga, and Mindfulness
Alternative therapies can be a valuable adjunct to medical and surgical management of endometriosis. In this section, we’ll explore some of the alternative therapies available, including acupuncture, yoga, and mindfulness, and their potential benefits in managing symptoms.
Acupuncture is a traditional Chinese medicine practice that involves inserting thin needles into specific points on the body. It has been found to be effective in reducing pain and inflammation associated with endometriosis. Yoga, on the other hand, is a mind-body practice that combines physical postures, breathing techniques, and meditation. It can help reduce stress and anxiety, which are common symptoms of endometriosis. Mindfulness, which involves being present and aware of one’s thoughts and feelings, can also be helpful in managing endometriosis symptoms. By practicing mindfulness, individuals with endometriosis can learn to better cope with pain and stress.
Living with Endometriosis: Coping Strategies and Support Resources
Endometriosis can be a challenging condition to live with, both physically and emotionally. In this section, we’ll explore some strategies for coping with endometriosis and the support resources available to women with the condition.
One of the most effective coping strategies for managing endometriosis is to maintain a healthy lifestyle. This includes eating a balanced diet, getting regular exercise, and getting enough sleep. Additionally, stress management techniques such as meditation, yoga, or therapy can help reduce the impact of endometriosis on mental health.
It’s also important for women with endometriosis to have a strong support system. This can include family, friends, and healthcare providers who understand the challenges of living with the condition. Support groups and online communities can also provide a sense of community and understanding for those with endometriosis.
Future Directions in Endometriosis Research: Advances in Diagnosis and Treatment
Endometriosis is an area of ongoing research, with significant progress being made in developing new diagnostic and treatment options. In this section, we’ll explore the latest developments in endometriosis research and what they could mean for women living with the condition.
Endometriosis has a long and complex history, but with advances in diagnosis and treatment, the outlook for women with the condition is improving. By understanding its causes, symptoms, and treatment options, women with endometriosis can take control of their health and lead happy, healthy lives.
One promising area of research in endometriosis is the use of non-invasive diagnostic tools, such as biomarkers and imaging techniques. These methods could potentially reduce the need for invasive procedures, such as laparoscopy, which is currently the gold standard for diagnosis. Additionally, researchers are exploring new treatment options, including targeted therapies and immunomodulators, which could provide more effective and personalized treatment for women with endometriosis.
Most Asked Questions
-
Can endometriosis be cured?
There is currently no cure for endometriosis, but symptoms can often be managed effectively with appropriate treatment. However, recurrence of symptoms after treatment is common, and long-term management may be necessary.
-
Are there specific medications to alleviate endometriosis ovulation pain?
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can be effective in reducing pain. Hormonal therapies, including birth control pills or GnRH agonists, may be prescribed to regulate the menstrual cycle and manage pain. Prescription pain medications may also be recommended for severe cases.
-
Can endometriosis lead to cancer?
While endometriosis is not cancer, there is a slightly increased risk of certain types of ovarian cancer in individuals with the condition. However, the overall risk is still relatively low.
-
Can endometriosis cause infertility?
Endometriosis can affect fertility by causing inflammation, scarring, and adhesions in the pelvic area, which may interfere with conception or implantation.
-
Can endometriosis ovarian cysts affect fertility?
Yes, endometriosis ovarian cysts can significantly impact fertility. The presence of these cysts, along with associated inflammation and scarring, can interfere with ovulation, fertilization, and implantation, making it more challenging for individuals to conceive.
-
Can endometriosis ovulation pain impact fertility?
While ovulation pain itself may not directly affect fertility, endometriosis, if left untreated, can lead to the formation of adhesions and scar tissue that may impact reproductive organs. Seeking early intervention and management can be crucial for those trying to conceive.
-
Does endometriosis always require surgery?
Surgery may be necessary to diagnose or treat endometriosis in some cases, but not all individuals with the condition will require surgery. Treatment options vary depending on the severity of symptoms and the individual's goals for managing the condition.
-
How Can Endometriosis Leg Pain Be Differentiated from Other Causes?
Diagnosis involves ruling out other conditions causing leg pain. Imaging, pelvic exams, and symptom analysis help discern whether endometriosis or unrelated factors contribute to the discomfort.
-
How are endometriosis ovarian cysts diagnosed?
Diagnosis typically involves a combination of medical history review, pelvic examination, imaging tests like ultrasound, and sometimes laparoscopy for definitive diagnosis.
-
How can diet help manage endometriosis symptoms?
Certain foods like fatty fish rich in omega-3 fatty acids and anti-inflammatory spices like turmeric can help reduce inflammation and alleviate pain associated with endometriosis. It’s also beneficial to focus on a diet that balances estrogen levels, avoiding dairy products that may exacerbate symptoms.





































