What Is Chlamydia?

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

Satadeepa is a Psychologist with 5 years of experience in the field of mental health and holds a Master's Degree in Clinical Psychology. Her areas of work interest and specialization include anxiety & mood disroders, relationship issues, self esteem development, grief, behavioural sleep medicine and sexual wellness.

Anoush Gomes is a seasoned Content Writer with over 10 years of experience, specializing in various writing styles such as medical content, creative writing, storytelling, and research papers. Anoush embarked on a unique journey, starting with pre-medical studies at the Dante Aligheri Academy and the University of Miami, where she earned a Bachelor's degree with a major in Biology and a minor in Psychology. Having pursued medical school and completed clinicals, Anoush transitioned to the world of medical content writing, where her passion for both healthcare and writing converged. Her writing skills encompass persuasive, narrative, expository, and descriptive styles, making complex medical concepts accessible to diverse audiences. Beyond her professional endeavors, Anoush is a multi-faceted individual with a rich tapestry of interests. A writer, artist, poet, avid reader, certified nerd, and hopeful author, she finds inspiration in the intersection of creativity and science. Whether crafting engaging medical narratives or weaving captivating stories, Anoush combines her diverse background and writing expertise to deliver compelling content that resonates with diverse audiences.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 16 April, 2024
- Article was updated as part of our commitment to diversity, equity, and inclusion.
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
What Is Chlamydia?
Chlamydia is a common sexually transmitted infection (STI) caused by the bacterium Chlamydia trachomatis. It is estimated that there are more than 131 million new cases of chlamydia every year worldwide, making it one of the most prevalent STIs.
Chlamydia can be transmitted through vaginal, anal, and oral sex, and can also be passed from mother to child during childbirth. Many people who have chlamydia may not show any symptoms, which is why it is often referred to as a “silent” infection. However, even without symptoms, chlamydia can cause serious complications if left untreated.
Types of Chlamydia
There are three main types of chlamydia: genital, ocular, and respiratory.
Genital Chlamydia
Genital chlamydia is the most common type of chlamydia and is transmitted through sexual contact with an infected person. It can affect both men and women and can lead to serious health problems if left untreated. In women, it can cause pelvic inflammatory disease, which can lead to infertility and chronic pelvic pain. In men, it can cause epididymitis, which is a painful swelling of the testicles that can lead to infertility.
Ocular Chlamydia
Ocular chlamydia is caused by the same bacterium that causes genital chlamydia, but it affects the eyes instead of the genitals. It is most commonly found in newborns who are exposed to the bacteria during delivery from an infected mother. Ocular chlamydia can cause conjunctivitis, which is an inflammation of the eye that can lead to scarring and blindness if left untreated.
Respiratory Chlamydia
Respiratory chlamydia is caused by a different strain of the Chlamydia trachomatis bacterium than the one that causes genital chlamydia. It is transmitted through the air and can cause pneumonia in newborns and adults. Respiratory chlamydia can also cause a type of sexually transmitted infection called lymphogranuloma venereum, which can lead to genital ulcers, rectal bleeding, and lymph node swelling.
Causes of Chlamydia
Sexual Contact
The primary cause of chlamydia is sexual contact with an infected partner. This includes vaginal, anal, and oral sex. The bacterium that causes chlamydia can be found in the semen and vaginal fluids of infected individuals. If you have unprotected sex with an infected person, you are at risk of contracting chlamydia.
Multiple Sexual Partners
Having multiple sexual partners raises your chances of getting chlamydia. This is because the more partners you have, the more likely you are to come into contact with someone who is infected. Additionally, having multiple sexual partners can make it more difficult to determine who infected you if you do become infected.
Unprotected Sex
Unprotected sex is a significant risk factor for chlamydia. Using a condom during sexual activity can significantly reduce your risk of contracting chlamydia. However, condoms are not 100% effective in preventing the spread of chlamydia. The best way to reduce your risk of contracting chlamydia is to practice abstinence or have a mutually monogamous sexual relationship with a partner who has tested negative for chlamydia.
Age and Gender
Young adults and teenagers are at an increased risk of contracting chlamydia. This is because they are more likely to engage in risky sexual behavior and have multiple sexual partners. Women are at an increased risk of contracting chlamydia compared to men. This is because the cervix is more vulnerable to infection compared to the urethra in men.
Personal Hygiene
Poor personal hygiene can increase your risk of contracting chlamydia. This is because the bacterium that causes chlamydia can survive outside the body for a short period. If you do not practice good personal hygiene, such as washing your hands regularly or wiping from front to back after using the bathroom, you may be at risk of contracting chlamydia.
Health Conditions
Certain health conditions can increase your risk of contracting chlamydia. For example, individuals with HIV or other sexually transmitted infections are at an increased risk of contracting chlamydia. Additionally, individuals with weakened immune systems may be more susceptible to contracting chlamydia.
Symptoms of Chlamydia
Many people actually don’t experience any symptoms, which is why it’s often called the “silent” STD. When symptoms do occur, they can include:
Painful Urination
One of the most common symptoms of chlamydia is painful urination, also known as dysuria. This occurs because the infection can cause inflammation of the urethra, the tube that carries urine from the bladder out of the body. The inflammation can cause a burning sensation when urine passes through the urethra.
Abnormal Vaginal or Penile Discharge
Another symptom of chlamydia is abnormal discharge from the penis or vagina. This discharge may be thin and watery or thick and yellowish in color. The reason behind this symptom is that the bacteria can infect the cells that line the cervix in women or the urethra in men. This can cause an overproduction of mucus, which leads to discharge.
Pain or Bleeding During Sex
Pain or bleeding during sex, also known as dyspareunia, is another symptom of chlamydia. This occurs because the infection can cause inflammation of the cervix or urethra, which can make intercourse painful. Additionally, the inflammation can cause small blood vessels to burst, leading to bleeding during or after sex.
Lower Abdominal Pain
Lower abdominal pain is a less common symptom of chlamydia, but it can occur in some cases. This pain can be mild or severe and may be accompanied by nausea or fever. The reason behind this symptom is that the bacteria can cause inflammation in the reproductive organs, such as the uterus or fallopian tubes in women, or the epididymis in men. This inflammation can lead to pain in the lower abdomen.
Testicular Pain
Men with chlamydia may also experience testicular pain, also known as epididymitis. This occurs when the infection spreads to the epididymis, a coiled tube that stores and carries sperm. The inflammation caused by the infection can cause pain and swelling in the testicles.
Rectal Pain, Discharge, or Bleeding
Chlamydia besides the other sources, can also be transmitted through anal sex which can cause inflammation of the rectum, leading to pain, discharge, or bleeding. The inflammation can also cause the rectum to become more susceptible to other infections, such as bacterial or viral infections.
Conjunctivitis
In rare cases, chlamydia can also cause conjunctivitis, also known as pink eye. This occurs when the bacteria infects the conjunctiva, the thin, clear layer of tissue that covers the white part of the eye and lines the inside of the eyelid. This can cause redness, itching, and discharge from the eye.
Risk Factors of Chlamydia
Unprotected sex
One of the biggest risk factors for chlamydia is unprotected sex. This means having sex without a condom or any other barrier method. Chlamydia is spread through the exchange of bodily fluids during sexual contact, so unprotected sex puts you at a higher risk of contracting the infection.
Multiple sexual partners
The more sexual partners you have, the higher the likelihood that one of them may be infected with chlamydia. Additionally, having multiple sexual partners can make it difficult to trace the source of the infection, making it more difficult to receive treatment.
Age
Young people aged 15-24 are at a higher risk of contracting chlamydia than older individuals. This is likely due to a combination of factors, including a lack of knowledge about safe sex practices, an increased likelihood of engaging in risky sexual behaviors, and a greater likelihood of having multiple sexual partners.
Gender
Women are at a higher risk of contracting chlamydia than men. This is partly because the female anatomy makes it easier for the bacteria to infect the reproductive system. Additionally, women may be less likely to experience symptoms of chlamydia, which can make it more difficult to diagnose and treat.
Previous STI diagnosis
If you have been diagnosed with an STI in the past, you may be at a higher risk of contracting chlamydia. This is because individuals who have had an STI in the past are the ones more likely to engage in risky sexual behaviors in general, which can increase their risk of contracting chlamydia.
Substance use
Substance use, particularly alcohol and drugs, can increase your risk of contracting chlamydia. This is because substance use can lead to engaging in risky sexual behaviors, where one is under the effect of intoxication and is unable to make an aware decision of practicing safe sex. They then might end up having unprotected sex or having multiple sexual partners.
Lack of access to healthcare
Individuals who lack access to healthcare, including those who do not have health insurance or live in rural areas with limited healthcare options, may be at a higher risk of contracting chlamydia. This is because they may not have access to regular STI screenings or may be less likely to seek medical attention if they experience symptoms of chlamydia.
Geographic location
Chlamydia rates can vary depending on geographic location. In general, urban areas and areas with higher population densities tend to have higher rates of chlamydia. This is likely due to a combination of factors, including a higher likelihood of engaging in risky sexual behaviors and greater access to healthcare resources.
Immunodeficiency
Individuals with weakened immune systems, such as those with HIV/AIDS or cancer, may be at a higher risk of contracting chlamydia. This is because a weakened immune system can make it more difficult for the body to fight off infections.
Types Of Bacteria That Can Cause Chlamydia
Chlamydia is caused by a bacterial organism called Chlamydia trachomatis. This organism is one of the most common sexually transmitted pathogens worldwide. It is a gram-negative bacteria that can cause a range of infections, including urethritis, cervicitis, pelvic inflammatory disease (PID), and conjunctivitis.
There are two main types of Chlamydia trachomatis bacteria: serovars D-K and serovars L1-L3. Serovars D-K are responsible for genital chlamydia, while serovars L1-L3 cause lymphogranuloma venereum (LGV). Let’s take a closer look at each of these bacteria and how they cause chlamydia.
Serovars D-K
Serovars D-K are the most common cause of chlamydia. These bacteria infect the genital tract of both men and women, and they can be transmitted through vaginal, anal, and oral sex. The bacteria live inside the cells of the infected person’s genital tract and can cause symptoms such as painful urination, discharge, and genital itching.
Chlamydia trachomatis serovars D-K can also cause PID (Pelvic Inflammatory Disease), a serious infection of the female reproductive organs, which can lead to infertility, chronic pelvic pain, and other complications if left untreated. In men, chlamydia can lead to epididymitis, a painful condition that can affect fertility.
Serovars L1-L3
Serovars L1-L3 cause lymphogranuloma venereum (LGV), a rare but serious form of chlamydia. LGV is more common in tropical and subtropical regions and can affect the lymph nodes in the groin area. It can also cause ulcers on the genitals and anus.
LGV is transmitted through sexual contact, including vaginal, anal, and oral sex. The bacteria can also be spread through contact with infected skin or mucous membranes. Symptoms of LGV may include painful, swollen lymph nodes, fever, and fatigue. If left untreated, LGV can cause permanent damage to the lymphatic system and lead to chronic swelling and pain in the genitals.
Testing For Chlamydia: What To Expect
There are several methods of testing for chlamydia, including urine tests, swab tests, and blood tests. The most commonly used tests are urine tests and swab tests.
Urine Tests
A urine test for chlamydia is a simple and painless procedure that can be done in a doctor’s office or at a clinic. The patient will be asked to provide a urine sample, which will then be sent to a laboratory for testing. The test looks for the presence of the bacterium Chlamydia trachomatis in the urine sample. This test is highly accurate, and results are usually available within a few days.
Swab Tests
A swab test for chlamydia is another common method of testing. During this test, a healthcare provider will use a swab to collect a sample of cells from the cervix in women or the urethra in men. The swab may also be used to collect a sample from the rectum or throat if those areas are at risk of infection. This procedure can be slightly uncomfortable, but it is not painful. The sample is then sent to a laboratory for testing. Results are usually available within a few days.
Blood Tests
Blood tests for chlamydia are less common than urine and swab tests, and they are not as accurate. Blood tests look for the presence of antibodies in the blood that are produced in response to a chlamydia infection. However, antibodies can remain in the blood for months or even years after an infection has cleared, which can lead to false-positive results. Therefore, blood tests are not recommended as the primary method of testing for chlamydia.
What to expect during the testing process?
Getting tested for chlamydia is a simple and straightforward process. The healthcare provider will explain the testing procedure and answer any questions the patient may have. Depending on the type of test, the patient may be asked to provide a urine sample or undergo a swab test. The healthcare provider will then send the sample to a laboratory for testing. Results are usually available within a few days.
It is important to note that testing for chlamydia is confidential. Healthcare providers are required by law to keep patient information private, and test results will not be shared without the patient’s consent.
Treatment of Chlamydia

There are various treatments available for chlamydia, the reasons behind each treatment, and offer an empathetic tone to help readers understand and cope with this STI.
Antibiotics
Antibiotics are the most common treatment for chlamydia. The medication is taken orally, usually in a single dose. Antibiotics work by killing the bacteria causing the infection. There are several types of antibiotics used to treat chlamydia, including azithromycin, doxycycline, and erythromycin.
While antibiotics can be effective in treating chlamydia, it is important to finish the entire course of medication as prescribed, even if symptoms improve or disappear. This ensures that all the bacteria are eradicated and helps prevent the development of antibiotic-resistant strains of chlamydia.
Partner Treatment
Since chlamydia is a sexually transmitted infection, it is important for sexual partners to be treated as well. Even if a partner does not have symptoms, they may still be infected and can transmit the infection to others.
Partner treatment involves encouraging partners to get tested and treated for chlamydia. This can be a difficult conversation to have, but it is important to be honest and empathetic when discussing the concern. It is also recommended to abstain from sexual activity until both partners have completed treatment.
Abstinence
Abstinence is another treatment option for chlamydia, especially for those who are not in a monogamous relationship or are unable to access medication. Abstinence involves refraining from any sexual activity, including vaginal, anal, and oral sex.
While abstinence is an effective way to prevent chlamydia and other STIs, it may not be a realistic option for everyone. It is important to practice safe sex, use condoms, and get tested regularly if you are sexually active.
Symptom Management
Chlamydia can cause a range of symptoms, including discharge, pain during urination, and rectal pain or discharge. Symptom management involves treating these symptoms to help alleviate discomfort and improve overall well-being.
Over-the-counter pain medication, such as ibuprofen, can help alleviate pain and reduce inflammation. It is also important to avoid sexual activity during treatment to prevent further irritation or discomfort.
Follow-Up Testing
After completing treatment, it is recommended to get tested again to ensure that the infection has been fully treated. Follow-up testing also helps identify any potential reinfections and allows for prompt treatment to prevent complications.
Relationship Between Chlamydia and Sexual Health
Sexual health is an integral part of an individual’s overall health and well-being. Unfortunately, sexually transmitted infections (STIs) are a common occurrence among sexually active individuals, and Chlamydia is one of the most prevalent STIs worldwide. According to the World Health Organization (WHO), it is estimated that 127 million new cases of Chlamydia occur annually, and the majority of cases are among young adults aged 15-24 years old.
Chlamydia is caused by the bacteria Chlamydia trachomatis, which can infect both men and women. The infection is transmitted through unprotected sexual contact, including vaginal, anal, or oral sex. It can also be passed from a pregnant woman to her baby during delivery.
Chlamydia can negatively affect sexual health in various ways, including:
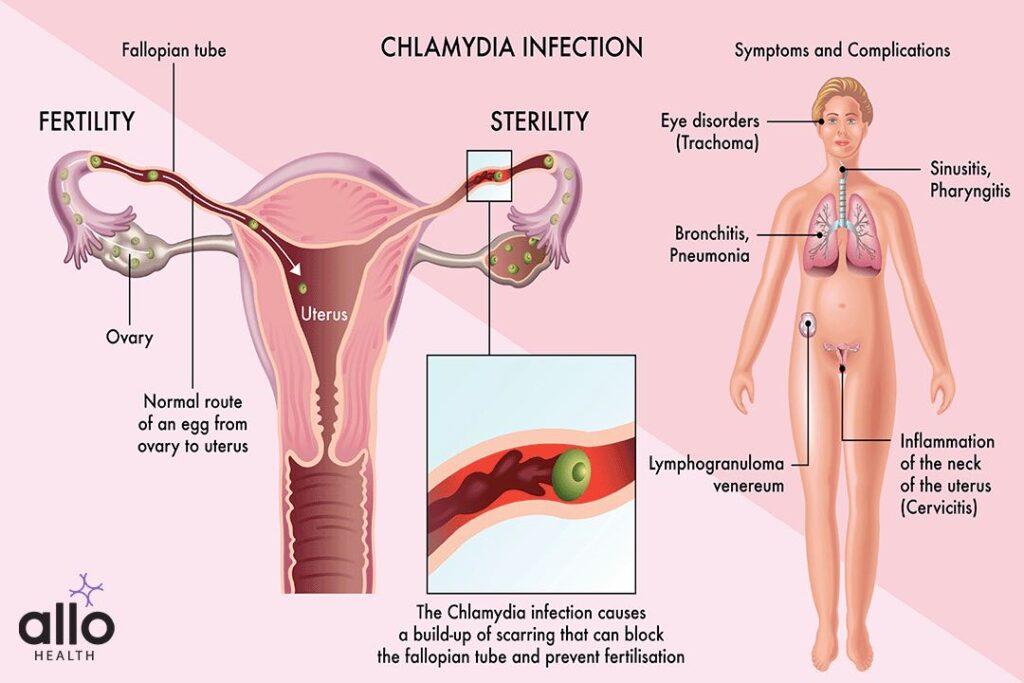
Infertility: Chlamydia can cause pelvic inflammatory disease (PID), which can result in fallopian tube scarring. This scarring can block the tubes and prevent fertilization of the egg, leading to infertility. In men, Chlamydia can cause epididymitis, which can lead to infertility by blocking the passage of sperm.
Increased risk of HIV: Chlamydia can increase the risk of acquiring or transmitting HIV during sexual contact. This is because Chlamydia can cause inflammation and small cuts or sores in the genital area, which can make it easier for HIV to enter the body.
Pain and discomfort: Chlamydia can cause pain and discomfort during sexual intercourse in both men and women. In women, the infection can cause vaginal discharge, itching, and burning, and in men, it can cause discharge from the penis, pain or burning during urination, and pain or swelling in the testicles.
Complications during pregnancy: Chlamydia can cause complications during pregnancy, such as premature birth, low birth weight, and even miscarriage. Infected pregnant women can also pass the infection to their baby during delivery, which can lead to eye infections and pneumonia in newborns.
It is important to note that Chlamydia can also cause infections in other parts of the body, such as the rectum and throat, which can lead to serious health concerns if left untreated.
How Can Chlamydia Affect Your Sex Life?
Physical Effects of Chlamydia on Your Sex Life
Chlamydia can have several physical effects on your sex life, ranging from mild discomfort to serious complications. These include:
Painful Sex
Chlamydia can cause inflammation and irritation in the genital area, leading to painful sex. This can be particularly uncomfortable for women, as it can cause pain during penetration and lead to discomfort after sex.
Infertility
In women, chlamydia can lead to scarring and damage to the reproductive system, potentially leading to infertility. This can be particularly devastating for those who hope to start a family in the future.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is a critical complication of chlamydia, particularly – it is an infection of the reproductive organs, which can cause severe pain, fever, and infertility.
Increased Risk of Other STIs
Chlamydia can increase your risk of contracting other STIs, such as gonorrhea and HIV. This is because the inflammation caused by chlamydia can create openings in the mucous membranes of the genitals, making it easier for other infections to take hold.
Emotional Effects of Chlamydia on Your Sex Life
In addition to physical effects, chlamydia can also have emotional effects on your sex life. These include:
Anxiety and Stress
Being diagnosed with an STI can be incredibly stressful and anxiety-inducing. Many people worry about how their diagnosis will affect their sex life and relationships, which can lead to increased stress and anxiety.
Relationship Strain
Chlamydia can put a strain on your relationship, particularly if your partner has also been infected. This can be especially difficult if you are not in an exclusive relationship or if you have to disclose your diagnosis to a new partner.
Stigma and Shame
Despite the fact that STIs are incredibly common, there is still a significant amount of stigma and shame surrounding them. Many people feel embarrassed or ashamed to talk about their diagnosis, which can lead to feelings of isolation, loneliness and poor self esteem.
What Doctor Do You Go To?
If you suspect that you might have chlamydia, it’s natural to feel anxious and uncertain about what steps to take next. One of the most pressing questions you may have is which doctor to see for diagnosis and treatment.
First and foremost, it’s important to understand that chlamydia is a sexually transmitted infection (STI) caused by the bacteria Chlamydia trachomatis. It is a common infection that can affect both men and women and can cause serious health complications if left untreated.
Now, let’s explore the different types of healthcare providers you can consult if you suspect you have chlamydia:
Primary Care Physician (PCP): If you have a primary care physician, they should be your first point of contact. PCPs are general practitioners who provide comprehensive medical care, including STI testing and treatment. They can diagnose chlamydia through a physical exam, urine test, or swab test. If the test comes back positive, they can prescribe antibiotics to treat the infection. They can also offer guidance on how to prevent future infections.
Gynecologist/Obstetrician (OB/GYN): Women who suspect they have chlamydia may prefer to see a gynecologist or obstetrician. These healthcare providers specialize in women’s reproductive health and can provide a more in-depth examination of the female reproductive system. They can also provide Pap tests, which can detect abnormal cells in the cervix that may indicate cervical cancer (which may not be the case always). Like PCPs, they can test for and treat chlamydia with antibiotics.
Urologist: Men who suspect they have chlamydia may prefer to see a urologist. These healthcare providers specialize in the male reproductive system and can provide a more detailed examination of the penis, testicles, and prostate. They can also perform a urethral swab to test for chlamydia. If the test comes back positive, they can prescribe antibiotics to treat the infection.
Telemedicine or consult online: Providers If you are unable to see a healthcare provider in person, telemedicine providers can be a convenient option. These healthcare providers offer virtual consultations and can prescribe antibiotics if needed. However, it’s important to note that telemedicine providers may not be able to perform physical examinations, so they may not be the best option if you are experiencing symptoms.
Prevention of Chlamydia
Prevention is key in reducing the incidence of Chlamydia and its negative impact on sexual health. Using barrier methods of contraception, such as condoms, during sexual contact can help reduce the risk of contracting Chlamydia and other STIs. Regular STI testing is also important, especially for individuals who are sexually active or have multiple partners.
Use Condoms
One of the most effective ways to prevent chlamydia is to use condoms during sex. Condoms act as a barrier, preventing the exchange of bodily fluids that can spread the infection. However, it is important to note that condoms are not 100% effective at preventing STIs, so it is still important to get regular STI screenings.
Get Regular STI Screenings
If you are sexually active, it is important to get regular STI screenings. This will help you detect any infections early on, so they can be treated before they cause serious health concerns. The CDC recommends that sexually active women under the age of 25 get tested for chlamydia every year.
Limit Your Number of Sexual Partners
The more sexual partners you have, the greater your risk of contracting chlamydia. Limiting your number of sexual partners can help reduce your risk of infection.
Talk to Your Partner(s)
It is important to have open and honest conversations with your sexual partner about your sexual health. If you are concerned about your partner’s sexual history, ask them to get tested for STIs before you have sex. If you or your partner have been diagnosed with chlamydia, it is important to abstain from sex until the infection has been treated.
Practice Good Hygiene
Practicing good hygiene can also help reduce your risk of contracting chlamydia. Make sure to wash your hands regularly, especially after using the bathroom or before and after sex. Avoid sharing towels or underwear with others, as this can increase your risk of infection.
Get Vaccinated
There is currently no vaccine available for chlamydia, but there is a vaccine available for the human papillomavirus (HPV). HPV is a common STI that can increase your risk of developing cervical cancer, and the vaccine can help protect against certain strains of the virus. By getting vaccinated against HPV, you can reduce your risk of developing cervical cancer, which is often caused by untreated chlamydia.
Avoid Alcohol and Drug Use
Alcohol and drug use can impair your judgment and increase your risk of engaging in risky sexual behaviors that can lead to STIs. Avoiding alcohol and drug use, or using them in moderation, can help reduce your risk of contracting chlamydia.
You Shouldn’t Be Embarrassed About Having Chlamydia
First and foremost, it’s important to remember that chlamydia is a bacterial infection, and it can happen to anyone who is sexually active. It is not a reflection of your character or your worth as a person. It is simply a result of having unprotected sex with someone who has the infection.
Additionally, chlamydia is highly treatable with antibiotics. In fact, the Centers for Disease Control and Prevention (CDC) recommends that all sexually active women under the age of 25 get tested for chlamydia annually, even if they don’t have any symptoms. This is because chlamydia often doesn’t cause any symptoms, and if left untreated, it can lead to serious health concerns like pelvic inflammatory disease (PID) and infertility.
By getting tested for chlamydia and seeking treatment if necessary, you are taking control of your sexual health and protecting yourself from potential complications down the line. There’s nothing embarrassing about being responsible and taking care of your body.
What You Can Do If You Think You Might Have Chlamydia
If you think you might have chlamydia, the first step is to get tested. Chlamydia tests are usually done by taking a urine sample or a swab from the genital area. You can get tested at your doctor’s office, a sexual health clinic, or even order a test kit online.
If your test comes back positive, don’t panic. As we mentioned earlier, chlamydia is easily treatable with antibiotics. Your doctor will prescribe a course of antibiotics, which you will need to take as directed to clear the infection. It’s important to follow your doctor’s instructions closely and finish the entire course of antibiotics, even if you start feeling better before you finish.
During your treatment, it’s important to avoid having sex until you have completed the entire course of antibiotics and your doctor has confirmed that the infection has cleared.
Incidence Of Chlamydia In India
India is the second most populous country in the world with a population of over 1.3 billion people. Despite the high burden of sexually transmitted infections (STIs) in India, there is limited data on the prevalence of chlamydia. According to a study published in the Indian Journal of Medical Microbiology, the prevalence of chlamydia in the general population of India ranges from 2.4% to 4.4%. However, the study also notes that there is a lack of large-scale, population-based studies on chlamydia in India, and the actual prevalence may be higher.
Chlamydia is more common among certain high-risk groups in India, including sex workers, men who have sex with men, and transgender individuals. A study published in the journal BMC Infectious Diseases found that the prevalence of chlamydia among female sex workers in India was 9.1%. Another study published in the journal Sexually Transmitted Diseases found that the prevalence of chlamydia among men who have sex with men in India was 6.7%.
Impact of Chlamydia on Public Health
Chlamydia can have serious health consequences if left untreated.
In women, untreated chlamydia can lead to pelvic inflammatory disease (PID), which can cause infertility and chronic pelvic pain. Chlamydia can also increase the risk of ectopic pregnancy, a potentially life-threatening condition in which a fertilized egg implants outside the uterus.
In men, chlamydia can lead to epididymitis, an inflammation of the epididymis that can cause pain and swelling in the scrotum.
Chlamydia can also increase the risk of acquiring and transmitting other sexually transmitted infections, including HIV. A study published in the Journal of Acquired Immune Deficiency Syndromes found that chlamydia infection was associated with a two-fold increased risk of HIV acquisition in men who have sex with men in India.
Chlamydia Vaccination
1. What is chlamydia vaccination?
Chlamydia vaccination is a type of vaccine that is designed to protect against chlamydia. The vaccine is currently in development and has not yet been approved for use. Researchers are working on developing a vaccine that will be effective in preventing chlamydia.
2. How does the chlamydia vaccine work?
The chlamydia vaccine works by stimulating the immune system to produce antibodies that can recognize and neutralize the chlamydia bacterium. If a person is exposed to chlamydia after receiving the vaccine, their immune system will be able to quickly recognize and attack the bacterium, preventing the infection from taking hold.
3. Who should get the chlamydia vaccine?
The chlamydia vaccine is still in development, so it is not yet available for use. Once the vaccine is approved, it will likely be recommended for individuals who are at high risk of contracting chlamydia. This includes sexually active individuals, especially those who have multiple sexual partners.
4. When will the chlamydia vaccine be available?
It’s difficult to say when the chlamydia vaccine will be available. Vaccines typically go through several stages of development and testing before they are approved for use. The chlamydia vaccine is currently in the early stages of development, and it may be several years before it is available for use.
5. How effective will the chlamydia vaccine be?
The effectiveness of the chlamydia vaccine is not yet known, as the vaccine is still in development. Researchers are working to develop a vaccine that will be effective in preventing chlamydia, but it’s too early to know for sure how effective the vaccine will be.
6. Will the chlamydia vaccine be a one-time shot or will it require booster shots?
It’s not yet clear whether the chlamydia vaccine will be a one-time shot or if it will require booster shots. The need for booster shots will depend on the effectiveness of the vaccine and how long the immunity it provides lasts.
7. Are there any side effects of the chlamydia vaccine?
The side effects of the chlamydia vaccine are not yet known, as the vaccine is still in development. However, vaccines in general can cause side effects such as soreness at the injection site, fever, and headache. These side effects are usually mild and go away on their own within a few days and are often common to other vaccination processes.
8. Can the chlamydia vaccine be used to treat chlamydia?
No, the chlamydia vaccine cannot be used to treat chlamydia once a person has already contracted the infection. The vaccine is designed to prevent chlamydia, not treat it.
9. Who should get a chlamydia vaccine?
A chlamydia vaccine would be recommended for anyone who is at risk of contracting chlamydia, especially sexually active individuals. However, until a vaccine is approved and available in India, the best way to prevent chlamydia is through safe sex practices such as using condoms and getting regular STI screenings
Frequently Asked Questions (FAQs)
1. How is Chlamydia Diagnosed?
Chlamydia can be diagnosed with a simple test that involves taking a swab from the infected area (such as the cervix or urethra) or a urine sample. The test is quick, painless, and can be done at a doctor’s office, clinic, or health department.
2. Can Chlamydia be Cured?
Yes, chlamydia can be cured with antibiotics. The most commonly prescribed antibiotics for chlamydia are azithromycin and doxycycline. It’s important to finish the entire course of antibiotics, even if you start feeling better before the medication is finished.
3. Can Chlamydia Come Back?
Yes, it’s possible for chlamydia to come back after it’s been treated. This is because you can still be infected with chlamydia even if you don’t have symptoms. It’s important to get tested again after finishing treatment to make sure the infection is gone.
4. Is there a chlamydia vaccine available in India?
Currently, there is no approved vaccine for chlamydia in India. However, research is ongoing to develop a safe and effective vaccine. Some studies have shown promising results in animal models, and clinical trials are underway in humans.
5. Where can I test for chlamydia vaccine in India?
- Private hospitals and clinics are an excellent option for testing for chlamydia in India. They have trained medical professionals who can conduct chlamydia tests and provide treatment if needed. Private hospitals and clinics are also more likely to have modern equipment and testing procedures than public hospitals.
- Public hospitals and clinics are another option for chlamydia testing in India. These facilities are often more affordable than private hospitals, and some even offer free testing services. However, they may have longer wait times, and the equipment and testing procedures may not be as modern as private hospitals.
- Online services are becoming increasingly popular in India for chlamydia testing. These services allow you to order a testing kit online, collect a sample at home, and then send it back to the laboratory for testing. Once the test results are available, you can receive them online, and if necessary, receive treatment as well from a registered health care professional.
References
- World Health Organization. (2021). Sexually transmitted infections (STIs). Retrieved from https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
- Centers for Disease Control and Prevention. (2022). Chlamydia – CDC fact sheet (detailed). Retrieved from https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm
- World Health Organization. (2019). Chlamydia. Retrieved from https://www.who.int/news-room/q-a-detail/chlamydia
- Healthline. (2022). Chlamydia: Symptoms, causes, and treatments. Retrieved from https://www.healthline.com/health/chlamydia
- American Sexual Health Association. (2022). Chlamydia. Retrieved from https://www.ashasexualhealth.org/stdsstis/chlamydia/
Bala M, Singh V. Chlamydia trachomatis infection in India: a review of the literature. Sex Health. 2012;9(2):111-117. doi:10.1071/SH11068
National AIDS Control Organisation. National Integrated Biological and Behavioural Surveillance (IBBS), India, 2014-15: State Fact Sheets. Ministry of Health and Family Welfare, Government of India; 2016.
- Reza-Paul S, Beattie T, Syed HU, et al. Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS. 2008;22 Suppl 5:S91-S100. doi:10.1097/01.aids.0000343760.71315.55
- Solomon MM, Mayer KH, Glidden DV, et al. Syphilis predicts HIV incidence among men and transgender women who have sex with men in a preexposure prophylaxis trial. Clin Infect Dis. 2014;59(7):1020-1026. doi:10.1093/cid/ciu447
- World Health Organization. Chlamydia trachomatis – Fact Sheet. https://www.who.int/news-room/fact-sheets/detail/chlamydia-trachomatis. Accessed March 15, 2023.
- Centers for Disease Control and Prevention. Chlamydia – CDC Fact Sheet. https://www.cdc.gov/std/chlamydia/stdfact-chlamydia-detailed.htm. Accessed March 15, 2023






































